From a MedPageToday online article:
 “Amyloid is important in initiating disease, but the actual damage in the brain is probably due to the accumulation of tau,” Holtzman told MedPage Today. “Normally, tau protein is inside cells, but there is more and more evidence suggesting that its spread to different parts of the brain is responsible for the progression of Alzheimer’s disease.”
“Amyloid is important in initiating disease, but the actual damage in the brain is probably due to the accumulation of tau,” Holtzman told MedPage Today. “Normally, tau protein is inside cells, but there is more and more evidence suggesting that its spread to different parts of the brain is responsible for the progression of Alzheimer’s disease.”
Two studies in January explored how sleep might be associated with Alzheimer’s tau pathology. The first, led by Brendan Lucey, MD, and David Holtzman, MD, both of Washington University in St. Louis, found that older adults who had less slow-wave sleep had higher levels of brain tau.
The findings, published in Science Translational Medicine, suggested that poor quality sleep in late life may signal deteriorating brain health.
Sleep patterns predicted amyloid and tau burden, reported Matthew Walker, PhD, of the University of California Berkeley, and co-authors, in June.



 “Our data showed that rates of accelerating blood pressure elevation were significantly higher in women than men, starting earlier in life,” said Cheng, the Erika J. Glazer Chair in Women’s Cardiovascular Health, who also serves as director of Cardiovascular Population Sciences at the Barbra Streisand Women’s Heart Center. “This means that if we define the hypertension threshold the exact same way, a 30-year old woman with high blood pressure is probably at higher risk for cardiovascular disease than a man with high blood pressure at the same age.”
“Our data showed that rates of accelerating blood pressure elevation were significantly higher in women than men, starting earlier in life,” said Cheng, the Erika J. Glazer Chair in Women’s Cardiovascular Health, who also serves as director of Cardiovascular Population Sciences at the Barbra Streisand Women’s Heart Center. “This means that if we define the hypertension threshold the exact same way, a 30-year old woman with high blood pressure is probably at higher risk for cardiovascular disease than a man with high blood pressure at the same age.”




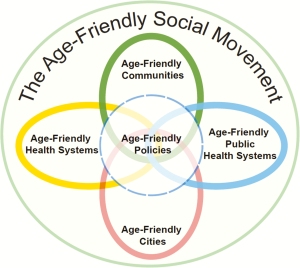 Becoming an Age-Friendly Health System entails reliably acting on a set of four evidence-based elements of high-quality care and services, known as the “4Ms,” for all older adults. When implemented together, the 4Ms represent a broad shift to focus on the needs of older adults:
Becoming an Age-Friendly Health System entails reliably acting on a set of four evidence-based elements of high-quality care and services, known as the “4Ms,” for all older adults. When implemented together, the 4Ms represent a broad shift to focus on the needs of older adults:

 Among older adults age 50–80, 43% had ever reviewed doctor ratings; 14% had reviewed ratings more than once in the past year, 19% had done so once in the past year, and 10% had reviewed ratings more than one year ago.
Among older adults age 50–80, 43% had ever reviewed doctor ratings; 14% had reviewed ratings more than once in the past year, 19% had done so once in the past year, and 10% had reviewed ratings more than one year ago. Ratings and reviews for nearly everything can be found online these days, including doctors. How are older adults using these ratings in their decisions about choosing doctors? In May 2019, the University of Michigan National Poll on Healthy Aging asked a
Ratings and reviews for nearly everything can be found online these days, including doctors. How are older adults using these ratings in their decisions about choosing doctors? In May 2019, the University of Michigan National Poll on Healthy Aging asked a
 The book follows the journey of a writer in search of wisdom, as he encounters twelve distinguished American men over 80 — including Paul Volcker, the former head of the Federal Reserve, and Denton Cooley, the world’s most famous heart surgeon. In these and other intimate conversations, the book explores and honors the particular way that each man faces four challenges of living a good old age: Am I still a man? Do I still matter? What is the meaning of my life? Am I loved?
The book follows the journey of a writer in search of wisdom, as he encounters twelve distinguished American men over 80 — including Paul Volcker, the former head of the Federal Reserve, and Denton Cooley, the world’s most famous heart surgeon. In these and other intimate conversations, the book explores and honors the particular way that each man faces four challenges of living a good old age: Am I still a man? Do I still matter? What is the meaning of my life? Am I loved?