Center for the Digital Future at USC Annenberg (Feb 19, 2020):
 Many Americans are willing to make significant personal tradeoffs to lower their health insurance rates or medical costs, such as agreeing to 24/7 personal monitoring or working with artificial intelligence instead of a human doctor, the Center for the Digital Future at the USC Annenberg School for Communication and Journalism finds.
Many Americans are willing to make significant personal tradeoffs to lower their health insurance rates or medical costs, such as agreeing to 24/7 personal monitoring or working with artificial intelligence instead of a human doctor, the Center for the Digital Future at the USC Annenberg School for Communication and Journalism finds.
Among the study’s findings:
- Nearly 1 in 4 Americans (24%) would work with an artificial intelligence-based technology if it lowered the cost of their health care.
- Most Americans (80%) think that access to health care is a basic right that should be available to all citizens regardless of their ability to pay. This is a view shared even by a majority of citizens who identify themselves as very conservative (56%).
- Significant percentages of Americans are willing to make profound lifestyle choices in exchange for lower insurance rates. For example, one-third of Americans would agree to 24/7 personal monitoring by insurance companies or health care professionals if their insurance rates were reduced.
- Twenty-one percent of Americans said they would stay in their current job if leaving it meant losing their current health coverage.
- Almost all Americans say health care is a key issue in the 2020 presidential election (92%).
- Even though Americans say they are satisfied with their current health insurance, they are open to alternatives. Thirty percent of Americans would consider buying health coverage from any company that offers lower costs, including a variety of non-insurance companies such as Amazon, Google, or Costco.


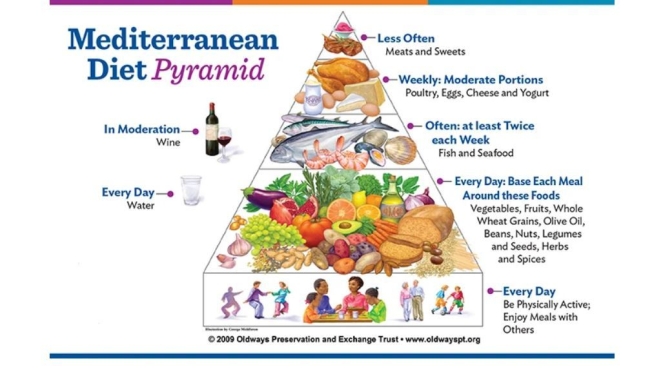
 We observed that increased adherence to the MedDiet modulates specific components of the gut microbiota that were associated with a reduction in risk of frailty, improved cognitive function and reduced inflammatory status.
We observed that increased adherence to the MedDiet modulates specific components of the gut microbiota that were associated with a reduction in risk of frailty, improved cognitive function and reduced inflammatory status.
 The association between poor overall sleep quality and greater consumption of added sugars observed in the current study aligns with previous findings that intakes of confectionary and sugar‐sweetened beverages were higher in middle‐aged Japanese women reporting poor, compared with good, sleep quality.
The association between poor overall sleep quality and greater consumption of added sugars observed in the current study aligns with previous findings that intakes of confectionary and sugar‐sweetened beverages were higher in middle‐aged Japanese women reporting poor, compared with good, sleep quality.
 In our opinion, the current recommendation to greatly increase consumption of dairy foods to 3 or more servings per day does not appear to be justified…When consumption of milk is low, the two nutrients of primary concern, calcium and vitamin D (which is of particular concern at higher latitudes), be obtained from other foods or supplements without the potential negative consequences of dairy foods.
In our opinion, the current recommendation to greatly increase consumption of dairy foods to 3 or more servings per day does not appear to be justified…When consumption of milk is low, the two nutrients of primary concern, calcium and vitamin D (which is of particular concern at higher latitudes), be obtained from other foods or supplements without the potential negative consequences of dairy foods. 
 In this analysis of commercially insured patients who had undergone elective surgery with an in-network surgeon at an in-network facility, approximately 1 in 5 received an out-of-network bill, with a mean potential balance bill of $2011.
In this analysis of commercially insured patients who had undergone elective surgery with an in-network surgeon at an in-network facility, approximately 1 in 5 received an out-of-network bill, with a mean potential balance bill of $2011.
 Intermittent fasting has salutary effects. Listen how Dr. Mark P. Mattson, co-author of a recent NEJM review on the topic, assesses the practice — and how he’s managed to skip breakfast for the past 30 years or so.
Intermittent fasting has salutary effects. Listen how Dr. Mark P. Mattson, co-author of a recent NEJM review on the topic, assesses the practice — and how he’s managed to skip breakfast for the past 30 years or so.
 Our findings suggest that LAN (low-level light at night) exposure increases the incidence of diabetes in a general elderly population. Further research involving a large cohort with new-onset diabetes is warranted to elucidate these findings.
Our findings suggest that LAN (low-level light at night) exposure increases the incidence of diabetes in a general elderly population. Further research involving a large cohort with new-onset diabetes is warranted to elucidate these findings.
 Steep incidence increases between 49 and 50 years of age are consistent with previously undetected colorectal cancers diagnosed via screening uptake at 50 years. These cancers are not reflected in observed rates of colorectal cancer in the SEER registries among individuals younger than 50 years. Hence, using observed incidence rates from 45 to 49 years of age alone to assess potential outcomes of earlier screening may underestimate cancer prevention benefits.
Steep incidence increases between 49 and 50 years of age are consistent with previously undetected colorectal cancers diagnosed via screening uptake at 50 years. These cancers are not reflected in observed rates of colorectal cancer in the SEER registries among individuals younger than 50 years. Hence, using observed incidence rates from 45 to 49 years of age alone to assess potential outcomes of earlier screening may underestimate cancer prevention benefits.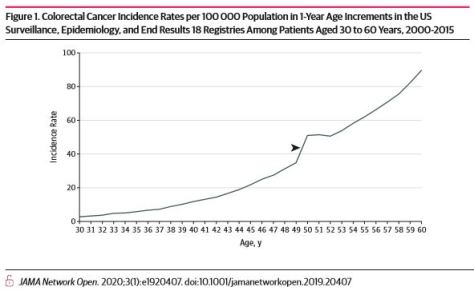
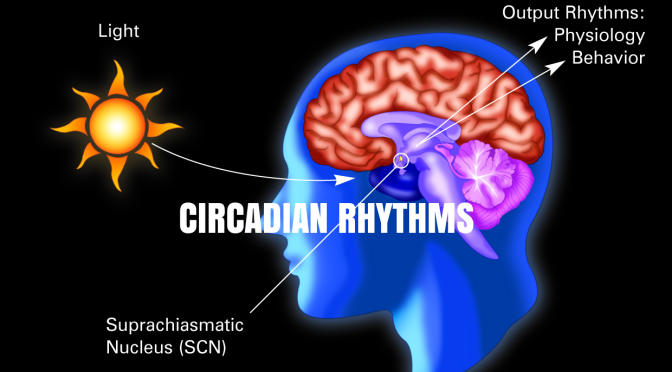
 By comparing the pancreatic cells of type 2 diabetic human donors with those of healthy people, researchers at the University of Geneva (UNIGE) and at the University Hospitals of Geneva (HUG), Switzerland, were able to demonstrate, for the first time, that the pancreatic islet cells derived from the Type 2 Diabetic human donors bear compromised circadian oscillators.
By comparing the pancreatic cells of type 2 diabetic human donors with those of healthy people, researchers at the University of Geneva (UNIGE) and at the University Hospitals of Geneva (HUG), Switzerland, were able to demonstrate, for the first time, that the pancreatic islet cells derived from the Type 2 Diabetic human donors bear compromised circadian oscillators.