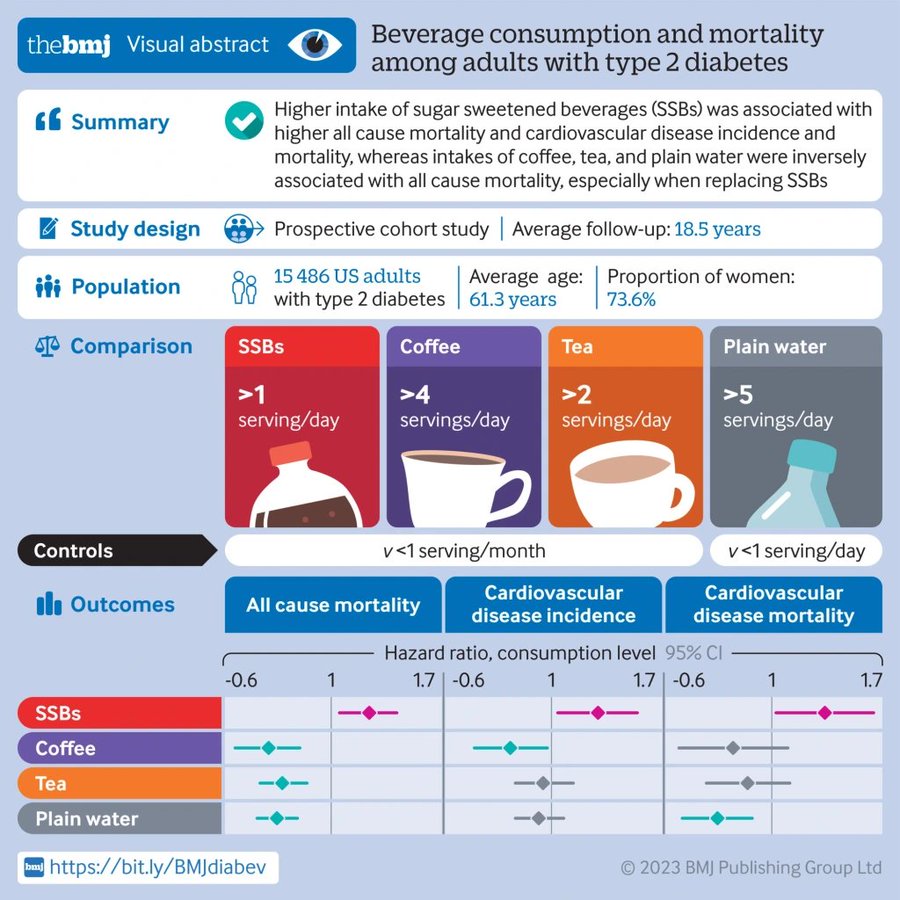
The BMJ (Published April 19, 2023) – Conclusions: Individual beverages showed divergent associations with all cause mortality and CVD outcomes among adults with type 2 diabetes. Higher intake of SSBs was associated with higher all cause mortality and CVD incidence and mortality, whereas intakes of coffee, tea, plain water, and low fat milk were inversely associated with all cause mortality. These findings emphasize the potential role of healthy choices of beverages in managing the risk of CVD and premature death overall in adults with type 2 diabetes.
Tag Archives: BMJ
Medicine: ‘Diabetes’ – Risks & Diagnosis (BMJ Podcast)

In this episode of the JIM Podcast, Editor-in-Chief Richard McCallum speaks with David Cistola of Texas Tech University Health Sciences Center El Paso about American Diabetes Month.
Health: ‘A Changing Climate, Changes Disease’
In recent decades, the worldwide burden of infectious disease has fallen, thanks to sanitation, hygiene, and prevention and control efforts. But the covid-19 pandemic shows how great a threat to global health remains – particularly as the climate crisis continues to affect disease spread and our response in myriad ways. Increasing temperatures are expanding the areas where diseases such as malaria and dengue thrive. More flooding and drought increases disease risk. Hygiene requires access to clean water. Further urbanization and migration related to climate change will also complicate prevention and control. The BMJ has published “The time is now” collection, calling for the strengthening of the global response to climate change and communicable disease. https://www.bmj.com/communicable-dise…
Infographic: Exercise For ‘Claudication’ (BMJ Study)

Exercise training is a safe, effective and low-cost intervention for improving walking ability in patients with IC. Additional benefits may include improvements in QoL, muscle strength and cardiorespiratory fitness. Clinical guidelines advocate supervised exercise training as a primary therapy for IC, with walking as the primary modality.
However, evidence is emerging for the role of various other modes of exercise including cycling and progressive resistance training to supplement walking training. In addition, there is emerging evidence for home-based exercise programmes. Revascularisation or drug treatment options should only be considered in patients if exercise training provides insufficient symptomatic relief.
Abstract
Peripheral artery disease (PAD) is caused by atherosclerotic narrowing of the arteries supplying the lower limbs often resulting in intermittent claudication, evident as pain or cramping while walking. Supervised exercise training elicits clinically meaningful benefits in walking ability and quality of life. Walking is the modality of exercise with the strongest evidence and is recommended in several national and international guidelines. Alternate forms of exercise such as upper- or lower-body cycling may be used, if required by certain patients, although there is less evidence for these types of programmes. The evidence for progressive resistance training is growing and patients can also engage in strength-based training alongside a walking programme. For those unable to attend a supervised class (strongest evidence), home-based or ‘self-facilitated’ exercise programmes are known to improve walking distance when compared to simple advice. All exercise programmes, independent of the mode of delivery, should be progressive and individually prescribed where possible, considering disease severity, comorbidities and initial exercise capacity. All patients should aim to accumulate at least 30 min of aerobic activity, at least three times a week, for at least 3 months, ideally in the form of walking exercise to near-maximal claudication pain.
Covid-19 Infographic: ‘Exercise Is Medicine’ (BMJ)


There are over 35,000,000 reported cases of COVID-19 disease and 1 000 000 deaths across more than 200 countries worldwide.1 With cases continuing to rise and a robust vaccine not yet available for safe and widespread delivery, lifestyle adaptations will be needed for the foreseeable future. As we try to contain the spread of the virus, adults are spending more time at home. Recent evidence2 suggests that physical activity levels have decreased by ~30% and sitting time has increased by ~30%. This is a major concern as physical inactivity and sedentary behaviour are risk factors3 for cardiovascular disease, obesity, cancer, diabetes, hypertension, bone and joint disease, depression and premature death.
To date, more than 130 authors from across the world have provided COVID-19-related commentary on these concerns. Many experts4 have emphasised the importance of increasing healthy living behaviours and others5 have indicated that we are now simultaneously fighting not one but two pandemics (ie, COVID-19, physical inactivity). Physical inactivity alone results in over 3 million deaths per year5 and a global burden of US$50 billion.6 Immediate action is required to facilitate physical activity during the COVID-19 pandemic because it is an effective form of medicine3 to promote good health, prevent disease and bolster immune function. Accordingly, widespread messaging to keep adults physically active is of paramount importance.
Several organisations including the WHO, American Heart Association and American College of Sports Medicine have offered initial suggestions and resources for engaging in physical activity during the COVID-19 pandemic. Expanding on these resources, our infographic aims to present a comprehensive illustration for promoting daily physical activity to the lay audience during the COVID-19 pandemic (figure 1). As illustrated, adults are spending more time at home, moving less and sitting more. Physical activity provides numerous health benefits, some of which may even help directly combat the effects of COVID-19. For substantial health benefits, adults should engage in 150–300 min of moderate-to-vigorous intensity physical activity each week and limit the time spent sitting. The recommended levels of physical activity are safely attainable even at home. Using a combination of both formal and informal activities, 150 min can be reached during the week with frequent sessions of physical activity spread throughout the day. Sedentary behaviour can be further reduced by breaking up prolonged sitting with short active breaks. In summary, this infographic offers as an evidence-based tool for public health officials, clinicians, educators and policymakers to communicate the importance of engaging in physical activity during the COVID-19 pandemic.
Infographic: ‘Functional Neurological Disorder’ – Signs & Symptoms (BMJ)

What you need to know
- Functional neurological disorder (FND) is associated with considerable distress and disability. The symptoms are not faked
- Diagnose FND positively on the basis of typical clinical features. It is not a diagnosis of exclusion
- FND can be diagnosed and treated in presence of comorbid, pathophysiologically defined disease
- Psychological stressors are important risk factors but are neither necessary nor sufficient for the diagnosis
Functional disorders are conditions whose origin arises primarily from a disorder of nervous system functioning rather than clearly identifiable pathophysiological disease—such as irritable bowel syndrome, fibromyalgia, and functional neurological disorder (FND)—they are the second commonest reason for new neurology consultations.1 FND is common in emergency settings,2 stroke,3 and rehabilitation services.4 It causes considerable physical disability and distress, and often places an economic burden both on patients and health services.5 Many clinicians have had little formal clinical education on the assessment and management of these disorders, and patients are often not offered potentially effective treatments.
Top Medical Podcasts: ‘Diverticular Disease’ (BMJ)
Colonic diverticulosis refers to herniation of the mucosa and submucosa through the muscular layer of the colonic wall and may be the result of colonic smooth muscle over-activity. Diverticular disease may be defined as any clinical state caused by symptoms pertaining to colonic diverticula and includes a wide-ranging spectrum from asymptomatic to severe and complicated disease.
Mohamed Thaha, Senior Lecturer & Lead Consultant in Colorectal Surgery, National Bowel Research Centre, Barts and The London School of Medicine and Dentistry, tells us more.
Top New Health Podcasts: ‘Flu Vaccine Season’ (BMJ)

With the annual flu season looming, GPs are anticipating a frenzy of vaccinations, perhaps more so than ever this year. As so many ‘flu and respiratory viruses circulate every year, and as the ‘flu vaccine is for one strain of influenza only, is the vaccine worth getting, and what are the risks associated with vaccinating vs. not vaccinating?
In this week’s episode, we discuss the high vaccine uptake in New Zealand, and the role that social distancing for COVID-19 may have played in their low numbers of seasonal flu. We also talk about whether or not the message we give to patients about the benefits and risks of vaccination is transparent enough, and how we might communicate better with them to allow them to make an informed decision. We feel pressure to increase vaccination rates, because we believe we are protecting people, but does the evidence support that?
Our guests: Nikki Turner is the director of the Immunisation Advisory Centre (IMAC) at the university of Auckland. She is an academic general practitioner, and a professor at the university. Jeff Kwong is a professor at the University of Toronto, and the interim director of the Centre for Vaccine Preventable Diseases at the university’s Dalla Lana School of Public Health. Newest Oldest Longest Shortest Random
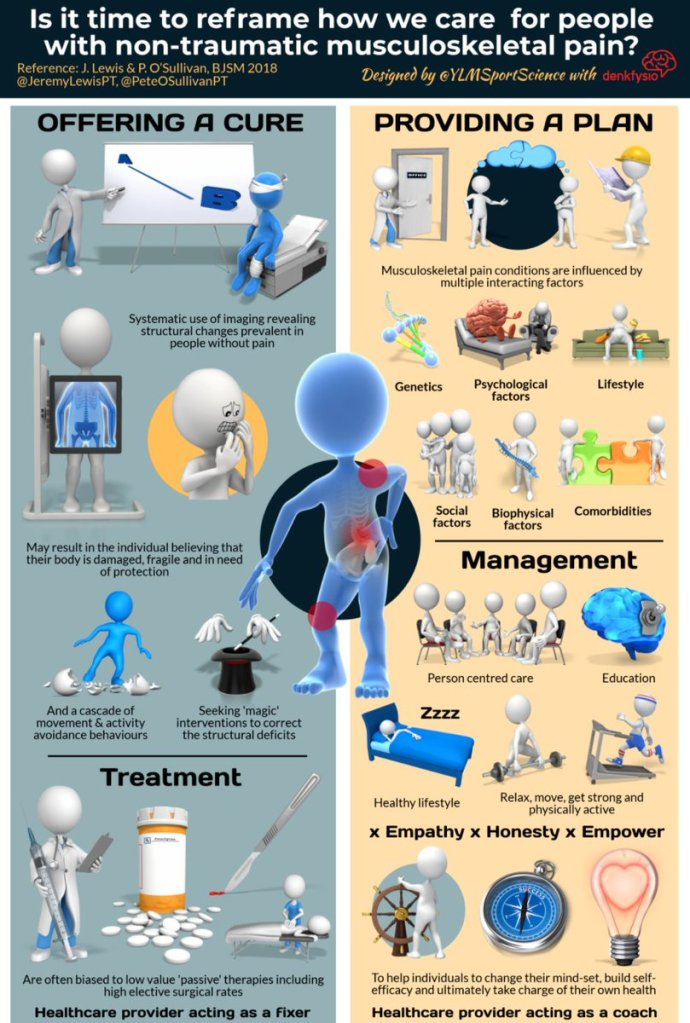
Infographic: Reframing Care For Non-Traumatic Musculoskeletal Pain
BMJ Podcast: What Is “Long-Covid” Syndrome?
Trisha Greenhalgh, professor of primary care health sciences at the University of Oxford has been a powerhouse of covid-19 evidence synthesis. She pulled together advice on doing remote consultations, on wearing masks to prevent spread, and a host of other information. She’s now turning her attention to “long-covid” – it’s becoming apparent that it’s not just an acute infection, patients are reporting chronic long term consequences of having the virus.
In this podcast, she describes what we know about long-covid, where the uncertainty lies, and what clinicians should be doing to help patients who are experiencing the symptoms.
Management of post-acute covid-19 in primary care https://www.bmj.com/content/370/bmj.m3026