
Tufts Health & Nutrition Letter (APRIL 2024): The new issue features 5 Ways to ID Ultraprocessed Foods; Should You Eat Gluten Free?; Q&A: Daily Food Choices and Myth: Carbs and Weight…

Tufts Health & Nutrition Letter (APRIL 2024): The new issue features 5 Ways to ID Ultraprocessed Foods; Should You Eat Gluten Free?; Q&A: Daily Food Choices and Myth: Carbs and Weight…
The Independent (February 21, 2024): Studies show that the average British person consumes more than half of their calories from ultra-processed foods. Their consumption can cause extreme health issues and early deaths, putting a massive strain on health services across the world.
An evaluation of global dietary guidelines highlights the need for clearer warnings on what common foods fall under the ‘UPF’ banner. Some of them may surprise you. Today, Decomplicated examines what exactly defines ultra-processed foods, the impact they have on both society and the environment, and what can you do to minimize your consumption of them.

Tufts Health & Nutrition Letter (JANUARY 2024): The new issue features ‘Healthy Lifestyle May Outweigh a Genetic Risk Factor for Heart Disease; How to Stick to Those Resolutions!; Check Your Nutrition Knowledge; Special Report – Expand Your Plant Palate; The Facts About Pea Protein; and more…
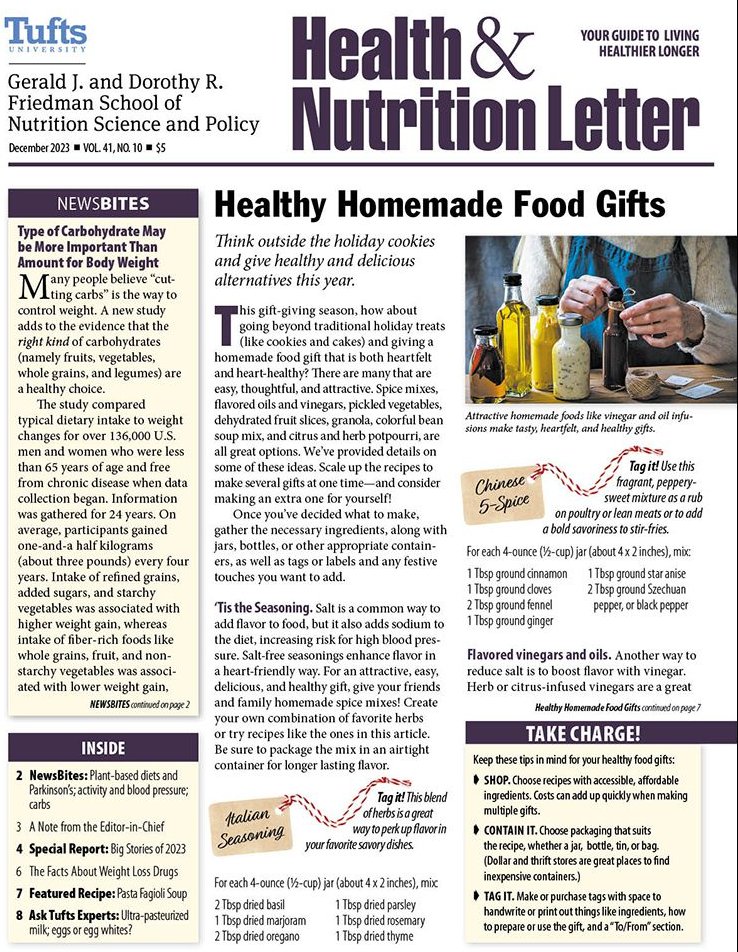

Tufts Health & Nutrition Letter (DECEMBER 2023): The new issue features Type of Carbohydrate May be More Important Than Amount for Body Weight; Beware of “Health-Washing” – Front package health claims can be misleading; Sweetened Beverages and Risk of Adverse Liver Outcomes…
Front-of-package health claims can be helpful—but they can also be misleading. Learn how to tell the difference.
Some health claims on packages or in advertising may be inappropriate or even misleading. This is sometimes referred to as “health-washing.”
Common Claims. Even FDA-approved claims (like organic, “non” or “free,” reduced, light, natural, and naturally raised) don’t guarantee the food or beverage is an overall healthy choice. Here are some red flags to look out for:

Tufts Health & Nutrition Letter (DECEMBER 2023):
This common condition increases the risk for type 2 diabetes, heart attack, and stroke. You may have it and not know it.
A little planning, prioritization, and creative problem solving can help you reach your behavior change goals.
Many of the ingredients in traditional Thanksgiving meals are native to the Americas.


Tufts Health & Nutrition Letter (August 2023):
There’s nothing like an icy drink or frozen treat to help tame summer swelter, keep you hydrated, quench thirst, and satisfy a sweet tooth. Unfortunately, cool treats are often over-processed and packed with added sugars. Keep your cool with less processed, fruit-forward icy drinks and treats that are as healthy …

Tufts Health & Nutrition Letter (July 2023): Food Allergy, or Intolerance?; Sugar substitute Erythritol associated with higher heart attack and stroke risks; Plant-based Cookouts; Create a Powerful Pantry, and more…
These terms are often used interchangeably, but there are important differences.
We asked a leading expert what you can do to stay strong and active at any age.
Trained as an oncological surgeon, Attia became interested in longevity because he saw that the “Four Horsemen” worked against it: diabetes, heart disease, cancer, and Alzheimer’s disease. All play a role in an unhealthy system, and all interrelate.

A data- and anecdote-rich invitation to live better, and perhaps a little longer, by making scientifically smart choices.
If you have Type 2 diabetes, then your chances of developing heart disease, cancer, and neurological disorders increases, and if your goal is to live well in old age, then it behooves you to change your ways in order to keep your insulin reception levels in the clear. How to do so?

Tufts Health & Nutrition Letter (April 2023)

Tufts Health & Nutrition Letter (March 2023):