From a The Lancet online editorial (Feb 3, 2020):
 Prevention represents the most cost-effective, long-term strategy for reducing the cancer burden and associated mortality. If provided with adequate information and support to adopt a healthy lifestyle, individuals can reduce their exposure to behavioural and dietary cancer risk factors by quitting smoking, maintaining a healthy BMI, cutting down on alcohol consumption, exercising more, and eating a healthy diet rich in fruit and vegetables.
Prevention represents the most cost-effective, long-term strategy for reducing the cancer burden and associated mortality. If provided with adequate information and support to adopt a healthy lifestyle, individuals can reduce their exposure to behavioural and dietary cancer risk factors by quitting smoking, maintaining a healthy BMI, cutting down on alcohol consumption, exercising more, and eating a healthy diet rich in fruit and vegetables.
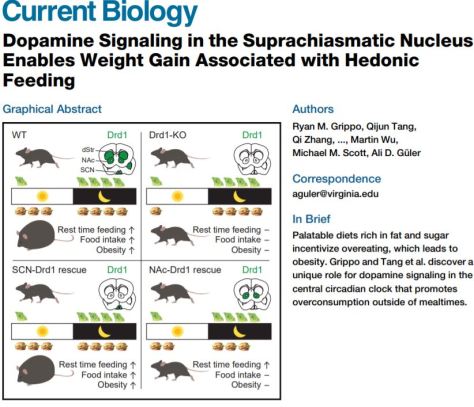
Although smoking is currently the major cause of preventable cancer cases and accounts for 22% of cancer deaths, a 2018 report from Cancer Research UK estimated that high BMI (overweight and obesity) now causes more cases of four common cancers (bowel, kidney, ovarian, and liver) in the UK than does smoking, and could overtake smoking as the biggest cause of cancer in women in the UK by 2043. According to WHO, in 2016, 1·9 billion adults around the world were overweight, of whom 650 million had obesity—triple the number in 1975. State-level projections for the USA paint an even bleaker picture going forward: by 2030, 48·9% of adults will have obesity; 24·2% of adults will have severe obesity; and severe obesity will be the most common BMI category among women, non-Hispanic black adults, and low-income adults. With such shocking statistics, the knock-on effect of the obesity epidemic for cancer prevention and control cannot be underestimated.


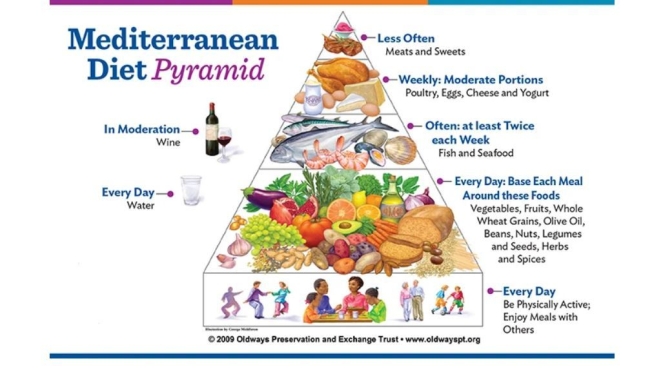
 We observed that increased adherence to the MedDiet modulates specific components of the gut microbiota that were associated with a reduction in risk of frailty, improved cognitive function and reduced inflammatory status.
We observed that increased adherence to the MedDiet modulates specific components of the gut microbiota that were associated with a reduction in risk of frailty, improved cognitive function and reduced inflammatory status.
 Intermittent fasting has salutary effects. Listen how Dr. Mark P. Mattson, co-author of a recent NEJM review on the topic, assesses the practice — and how he’s managed to skip breakfast for the past 30 years or so.
Intermittent fasting has salutary effects. Listen how Dr. Mark P. Mattson, co-author of a recent NEJM review on the topic, assesses the practice — and how he’s managed to skip breakfast for the past 30 years or so.
 There are many named diets that receive a great deal of attention. But what are they and do they work? David Heber, MD, PhD, from the UCLA Center for Human Nutrition explains these diets.
There are many named diets that receive a great deal of attention. But what are they and do they work? David Heber, MD, PhD, from the UCLA Center for Human Nutrition explains these diets.

 Our findings suggest that promotion of a healthy lifestyle would help to reduce the healthcare burdens through lowering the risk of developing multiple chronic diseases, including cancer, cardiovascular disease, and diabetes, and extending disease-free life expectancy. Public policies for improving food and the physical environment conducive to adopting a healthy diet and lifestyle, as well as relevant policies and regulations (for example, smoking ban in public places or trans-fat restrictions), are critical to improving life expectancy, especially life expectancy free of major chronic diseases.
Our findings suggest that promotion of a healthy lifestyle would help to reduce the healthcare burdens through lowering the risk of developing multiple chronic diseases, including cancer, cardiovascular disease, and diabetes, and extending disease-free life expectancy. Public policies for improving food and the physical environment conducive to adopting a healthy diet and lifestyle, as well as relevant policies and regulations (for example, smoking ban in public places or trans-fat restrictions), are critical to improving life expectancy, especially life expectancy free of major chronic diseases.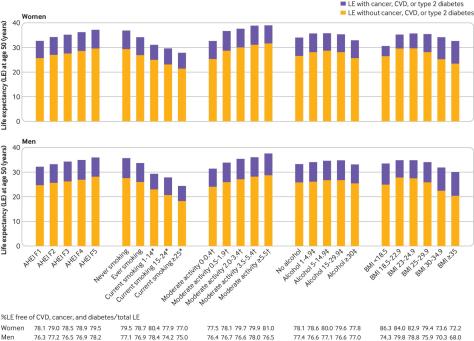

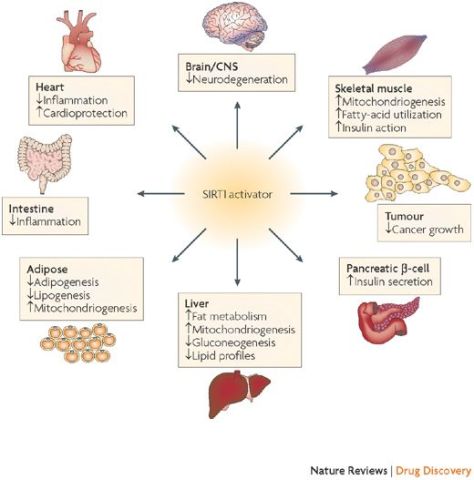
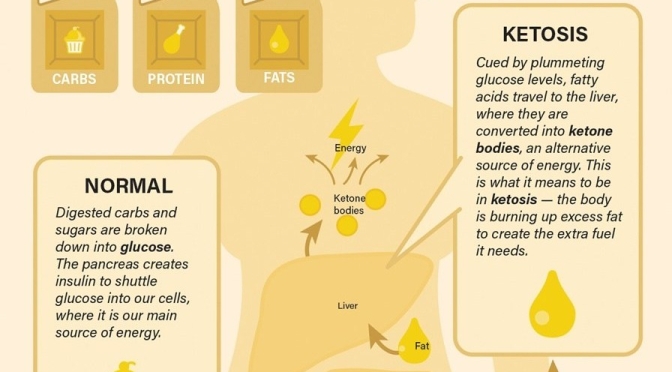
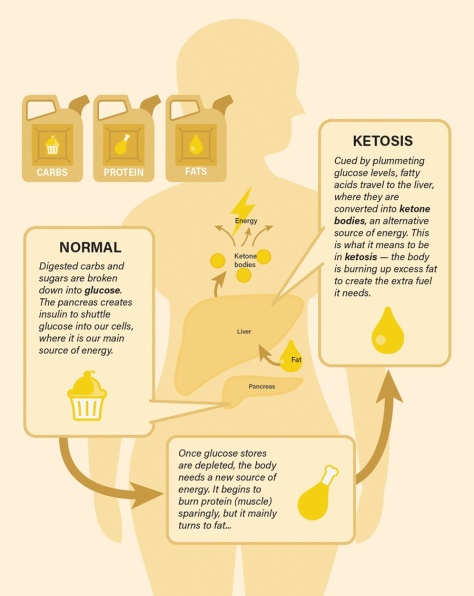
 to a paper Mattson and colleagues published in February in the experimental biology journal FASEB. In humans, fasting for 12 hours or more drops the levels of glycogen, a form of cellular glucose. Like changing to a backup gas tank, the body switches from glucose to fatty acids, a more efficient fuel. The switch generates the production of ketones, which are energy molecules that are made in the liver. “When the fats are mobilized and used to produce ketones, we think that is a key factor in accruing the health benefits,” says Mattson.
to a paper Mattson and colleagues published in February in the experimental biology journal FASEB. In humans, fasting for 12 hours or more drops the levels of glycogen, a form of cellular glucose. Like changing to a backup gas tank, the body switches from glucose to fatty acids, a more efficient fuel. The switch generates the production of ketones, which are energy molecules that are made in the liver. “When the fats are mobilized and used to produce ketones, we think that is a key factor in accruing the health benefits,” says Mattson.