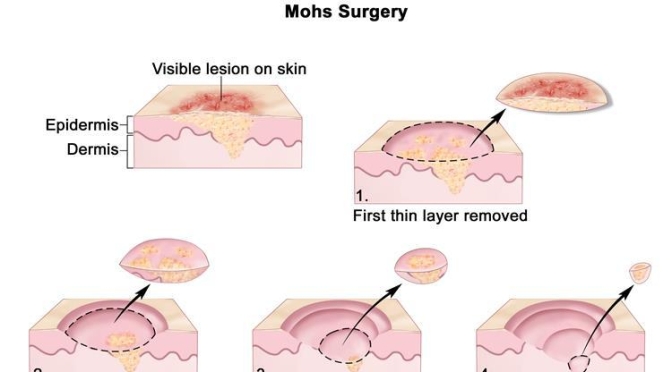
Named after the late Frederic Mohs, M.D., Mohs micrographic surgery is a highly precise excision technique in which the cancer is removed in stages, one tissue layer at a time. After each removal step, the layer is examined under a microscope to determine whether cancer remains in the patient’s skin and, if present, where exactly it is located so that the surgeon can pinpoint where to remove the remaining skin cancer. This allows for the smallest scar and best cosmetic result.
Category Archives: Aging
Health Infographics: How Exercise Creates “New Neurons In Aging Brains”
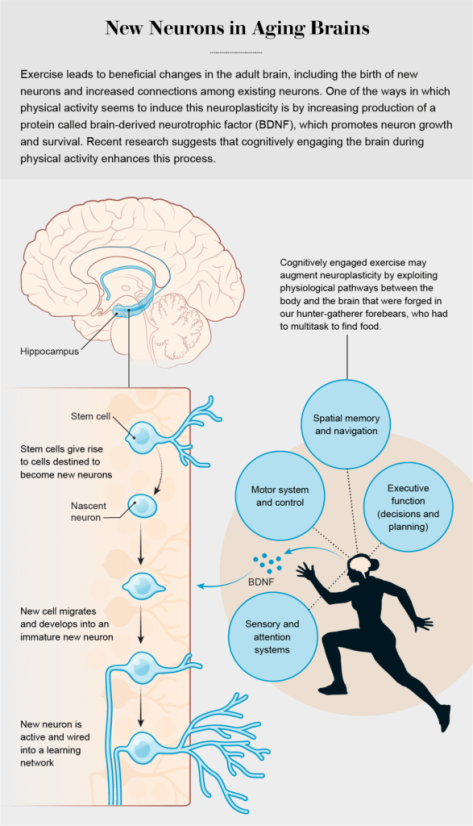

Researchers have also documented clear links between aerobic exercise and benefits to other parts of the brain, including expansion of the prefrontal cortex, which sits just behind the forehead. Such augmentation of this region has been tied to sharper executive cognitive functions, which involve aspects of planning, decision-making and multitasking—abilities that, like memory, tend to decline with healthy aging and are further degraded in the presence of Alzheimer’s. Scientists suspect that increased connections between existing neurons, rather than the birth of new neurons, are responsible for the beneficial effects of exercise on the prefrontal cortex and other brain regions outside the hippocampus.
Video Interviews: Neuroscientist Daniel Levitin On Aging Well (PBS)
As a neuroscientist, professor emeritus of psychology, musician and best-selling author, Daniel Levitin has extensively studied the brain and its impact on aging. His latest book, “Successful Aging,” explores the questions: what happens in the brain as we age and what are the keys to aging well? NewsHour Weekend’s Christopher Booker recently spoke to Levitin to learn more.
New Study: “Five Healthy Habits” For Diet, Exercise, BMI, Smoking & Alcohol” Lower Chronic Disease, Raise Lifespan (Harvard)
From a BMJ online article:
We derived a healthy lifestyle score based on information on five lifestyle factors—diet, smoking, physical activity, alcohol consumption, and body mass index (BMI).
 Our findings suggest that promotion of a healthy lifestyle would help to reduce the healthcare burdens through lowering the risk of developing multiple chronic diseases, including cancer, cardiovascular disease, and diabetes, and extending disease-free life expectancy. Public policies for improving food and the physical environment conducive to adopting a healthy diet and lifestyle, as well as relevant policies and regulations (for example, smoking ban in public places or trans-fat restrictions), are critical to improving life expectancy, especially life expectancy free of major chronic diseases.
Our findings suggest that promotion of a healthy lifestyle would help to reduce the healthcare burdens through lowering the risk of developing multiple chronic diseases, including cancer, cardiovascular disease, and diabetes, and extending disease-free life expectancy. Public policies for improving food and the physical environment conducive to adopting a healthy diet and lifestyle, as well as relevant policies and regulations (for example, smoking ban in public places or trans-fat restrictions), are critical to improving life expectancy, especially life expectancy free of major chronic diseases.
The average life expectancy in the world has increased substantially in the past few decades. The aging of the population has led to a high prevalence of chronic diseases such as diabetes, cardiovascular disease, and cancer. Although people live longer, older individuals often live with disabilities and chronic diseases. People with chronic diseases including cancer, cardiovascular disease, and diabetes have a shorter life expectancy than do their peers without these chronic conditions. Estimates of the loss in life years due to these chronic conditions range from 7.5 to 20 years, depending on the methods used and the characteristics of the study population.
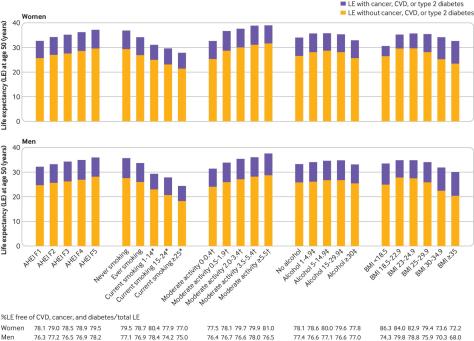
Modifiable lifestyle factors including smoking, physical activity, alcohol intake, body weight, and diet quality affect both total life expectancy and incidence of chronic diseases. Studies have shown that smoking, inactivity, poor diet quality, and heavy alcohol consumption contribute up to 60% of premature deaths and 7.4-17.9 years’ loss in life expectancy. Nevertheless, little research has looked at how a combination of multiple lifestyle factors may relate to life expectancy free from the major diseases of diabetes, cardiovascular disease, and cancer.
Senior Healthcare: The Challenges Of Safely “Aging In Place” (Video)
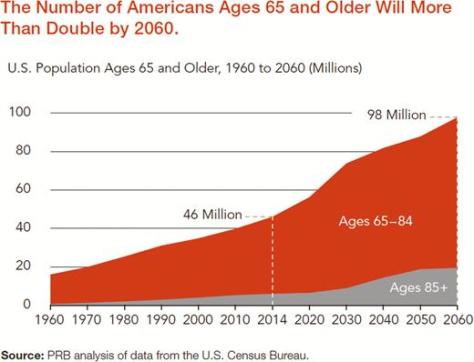
The 65-and-older population is the fastest-growing age group in the world. In this video, Stony Brook experts discuss the challenges facing this burgeoning population and their caregivers, and the technology that can facilitate happy, healthy and safe aging.
Innovation In Aging: “Creating an Age-Friendly Public Health System”
From an Innovation In Aging online release:
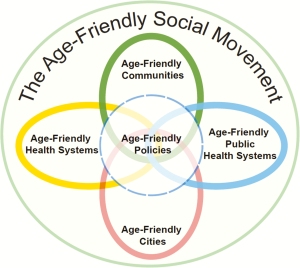 Becoming an Age-Friendly Health System entails reliably acting on a set of four evidence-based elements of high-quality care and services, known as the “4Ms,” for all older adults. When implemented together, the 4Ms represent a broad shift to focus on the needs of older adults:
Becoming an Age-Friendly Health System entails reliably acting on a set of four evidence-based elements of high-quality care and services, known as the “4Ms,” for all older adults. When implemented together, the 4Ms represent a broad shift to focus on the needs of older adults:
- (1) What Matters: Know and align care with each older adult’s specific health outcome goals and care preferences including, but not limited to, end-of-life care and across settings of care;
- (2) Medication: If medication is necessary, use Age-Friendly medication that does not interfere with What Matters to the older adult, Mobility, or Mentation across settings of care;
- (3) Mentation: Prevent, identify, treat, and manage dementia, depression, and delirium across settings of care; and
- (4) Mobility: Ensure that older adults move safely every day to maintain function and do What Matters
The Age-Friendly Health Systems movement, initiated in 2017, recognizes that an all-in, national response is needed to embrace the health and well-being of the growing older adult population. Like public health, health systems, including payers, hospitals, clinics, community-based organizations, nursing homes, and home health care, need to adopt a new way of thinking that replaces unwanted care and services with aligned interventions that respect older adults’ goals and preferences. Becoming an Age-Friendly Health System entails reliably acting on a set of four evidence-based elements of high-quality care and services, known as the “4Ms,” for all older adults.
Essays: 61-Year Old Canadian Writer Don Gillmor Reflects On Baby Boomers (Maclean’s)
From a Maclean’s Magazine online essay (01/08/20):

Boomers tore down institutions—divorce rates went up, churchgoing went down. We demonized the corporations that previous generations had venerated, though we bought their products in record numbers, our idealism blurring with the search for the perfect pair of jeans. We wanted it all. In place of institutions, we created the cult of the individual, our own particular Frankenstein.
So much of our music comes back to us in unfortunate ways, Dylan’s anthems barely recognizable in sappy orchestral arrangements that fill the hours we spend on hold. And we seem to be permanently on hold these days. We are between 55 and 73 years old now, still defining this as middle age, still a potent economic force because of our numbers, controlling 70 per cent of disposable income, though it feels to many of us that we have already disposed of it. Still, we bought houses when they were vaguely affordable. And politicians still cater to us because we vote en masse. However, we are largely left out of the cultural conversation, as music and social media continues to evolve, always leaving us one app behind the curve.

Health: “Multimorbidity” Is Rising, Creating Greater Demand For “Cluster Medicine” Expertise (BMJ)
From a The BMJ online editorial:
 The proportion of patients who have two or more medical conditions simultaneously is, however, rising steadily. This is currently termed multimorbidity, although patient groups prefer the more intuitive “multiple health conditions.” In high income countries, multimorbidity is mainly driven by age, and the proportion of the population living with two or more diseases is steadily increasing because of demographic change. This trend will continue.
The proportion of patients who have two or more medical conditions simultaneously is, however, rising steadily. This is currently termed multimorbidity, although patient groups prefer the more intuitive “multiple health conditions.” In high income countries, multimorbidity is mainly driven by age, and the proportion of the population living with two or more diseases is steadily increasing because of demographic change. This trend will continue.
Cluster medicine
The cluster around diabetes is a good example, with the common serious disease affecting the heart, nervous system, skin, peripheral vasculature, and eyes. Diabetologists already provide care for the cluster of multiorgan diseases around diabetes, and some specialties, such as geriatrics or general practice, have multimorbidity at their heart. For most, however, training and service organisation are not optimised to face a multimorbidity dominated future.
The shift includes moving from thinking about multimorbidity as a random assortment of individual conditions to recognising it as a series of largely predictable clusters of disease in the same person. Some of these clusters will occur by chance alone because individuals are affected by a variety of commonly occurring diseases. Many, however, will be non-random because of common genetic, behavioural, or environmental pathways to disease. Identifying these clusters is a priority and will help us to be more systematic in our approach to multimorbidity.
Medical Care: 43% Of Older Adults Review Doctor Ratings Online
From a National Poll on Aging (Univ. of Michigan) online release:
 Among older adults age 50–80, 43% had ever reviewed doctor ratings; 14% had reviewed ratings more than once in the past year, 19% had done so once in the past year, and 10% had reviewed ratings more than one year ago.
Among older adults age 50–80, 43% had ever reviewed doctor ratings; 14% had reviewed ratings more than once in the past year, 19% had done so once in the past year, and 10% had reviewed ratings more than one year ago.
Among older adults who had looked up doctor ratings within the past year, 65% read reviews of a doctor they were considering, 34% read reviews to find a new doctor, and 31% read reviews for a doctor they had already seen.
 Ratings and reviews for nearly everything can be found online these days, including doctors. How are older adults using these ratings in their decisions about choosing doctors? In May 2019, the University of Michigan National Poll on Healthy Aging asked a
Ratings and reviews for nearly everything can be found online these days, including doctors. How are older adults using these ratings in their decisions about choosing doctors? In May 2019, the University of Michigan National Poll on Healthy Aging asked a
national sample of adults age 50–80 about their use and perceptions of online doctor ratings.
Books On Aging: “Old Man Country” – Thomas R. Cole
 The book follows the journey of a writer in search of wisdom, as he encounters twelve distinguished American men over 80 — including Paul Volcker, the former head of the Federal Reserve, and Denton Cooley, the world’s most famous heart surgeon. In these and other intimate conversations, the book explores and honors the particular way that each man faces four challenges of living a good old age: Am I still a man? Do I still matter? What is the meaning of my life? Am I loved?
The book follows the journey of a writer in search of wisdom, as he encounters twelve distinguished American men over 80 — including Paul Volcker, the former head of the Federal Reserve, and Denton Cooley, the world’s most famous heart surgeon. In these and other intimate conversations, the book explores and honors the particular way that each man faces four challenges of living a good old age: Am I still a man? Do I still matter? What is the meaning of my life? Am I loved?
We aspire to live in a country where old men are celebrated as vital elders but not demeaned if they become ill and dependent. We aspire to maintain health as well as maintain dignity and fulfillment in frailty. Old Man Country helps readers see and imagine these possibilities for themselves.
Review of book in Houston Chronicle
Readers will come to see how each man — even the most famous — faces universal challenges. Personal stories about work, love, sexuality, and hope mingle with stories about illness, loss and death. This book will strengthen each of us as we and our loved ones anticipate and navigate our way through the passages of old age.