From a The BMJ online editorial:
 The proportion of patients who have two or more medical conditions simultaneously is, however, rising steadily. This is currently termed multimorbidity, although patient groups prefer the more intuitive “multiple health conditions.” In high income countries, multimorbidity is mainly driven by age, and the proportion of the population living with two or more diseases is steadily increasing because of demographic change. This trend will continue.
The proportion of patients who have two or more medical conditions simultaneously is, however, rising steadily. This is currently termed multimorbidity, although patient groups prefer the more intuitive “multiple health conditions.” In high income countries, multimorbidity is mainly driven by age, and the proportion of the population living with two or more diseases is steadily increasing because of demographic change. This trend will continue.
Cluster medicine
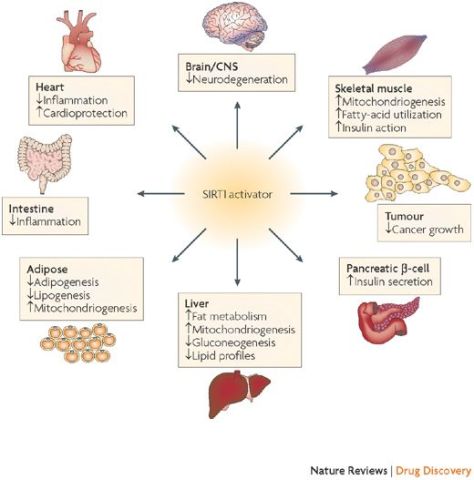
The cluster around diabetes is a good example, with the common serious disease affecting the heart, nervous system, skin, peripheral vasculature, and eyes. Diabetologists already provide care for the cluster of multiorgan diseases around diabetes, and some specialties, such as geriatrics or general practice, have multimorbidity at their heart. For most, however, training and service organisation are not optimised to face a multimorbidity dominated future.
The shift includes moving from thinking about multimorbidity as a random assortment of individual conditions to recognising it as a series of largely predictable clusters of disease in the same person. Some of these clusters will occur by chance alone because individuals are affected by a variety of commonly occurring diseases. Many, however, will be non-random because of common genetic, behavioural, or environmental pathways to disease. Identifying these clusters is a priority and will help us to be more systematic in our approach to multimorbidity.





 Among older adults age 50–80, 43% had ever reviewed doctor ratings; 14% had reviewed ratings more than once in the past year, 19% had done so once in the past year, and 10% had reviewed ratings more than one year ago.
Among older adults age 50–80, 43% had ever reviewed doctor ratings; 14% had reviewed ratings more than once in the past year, 19% had done so once in the past year, and 10% had reviewed ratings more than one year ago. Ratings and reviews for nearly everything can be found online these days, including doctors. How are older adults using these ratings in their decisions about choosing doctors? In May 2019, the University of Michigan National Poll on Healthy Aging asked a
Ratings and reviews for nearly everything can be found online these days, including doctors. How are older adults using these ratings in their decisions about choosing doctors? In May 2019, the University of Michigan National Poll on Healthy Aging asked a


 WHO’s definition of health is famously “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity”. One of the oldest medical texts we know of, The Science of Medicine attributed to Hippocrates, sets out the goal of medicine in comparable terms: “the complete removal of the distress of the sick”.
WHO’s definition of health is famously “a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity”. One of the oldest medical texts we know of, The Science of Medicine attributed to Hippocrates, sets out the goal of medicine in comparable terms: “the complete removal of the distress of the sick”.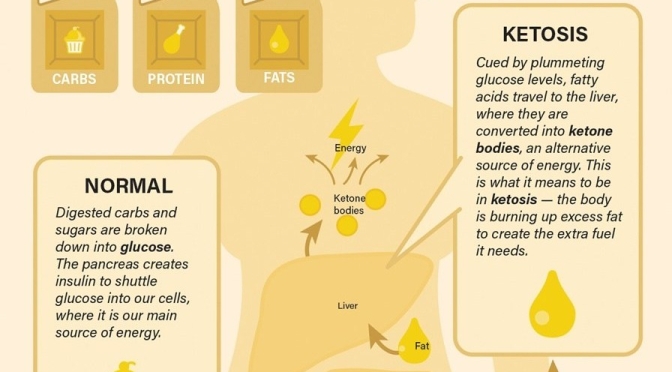
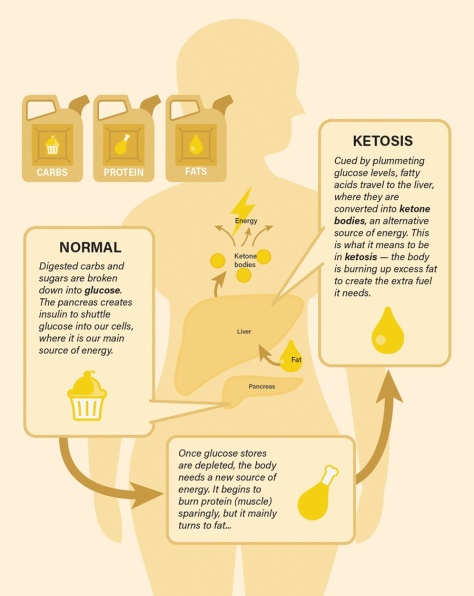
 to a paper Mattson and colleagues published in February in the experimental biology journal FASEB. In humans, fasting for 12 hours or more drops the levels of glycogen, a form of cellular glucose. Like changing to a backup gas tank, the body switches from glucose to fatty acids, a more efficient fuel. The switch generates the production of ketones, which are energy molecules that are made in the liver. “When the fats are mobilized and used to produce ketones, we think that is a key factor in accruing the health benefits,” says Mattson.
to a paper Mattson and colleagues published in February in the experimental biology journal FASEB. In humans, fasting for 12 hours or more drops the levels of glycogen, a form of cellular glucose. Like changing to a backup gas tank, the body switches from glucose to fatty acids, a more efficient fuel. The switch generates the production of ketones, which are energy molecules that are made in the liver. “When the fats are mobilized and used to produce ketones, we think that is a key factor in accruing the health benefits,” says Mattson.
 “This is an entirely new approach with no current treatments able to change scar in this way,” says Associate Professor James Chong who led the research. “By improving cardiac function and scar formation following heart attack, treatment with rhPDGF-AB led to an overall increase in survival rate in our study.”
“This is an entirely new approach with no current treatments able to change scar in this way,” says Associate Professor James Chong who led the research. “By improving cardiac function and scar formation following heart attack, treatment with rhPDGF-AB led to an overall increase in survival rate in our study.”
 Hundreds of miles south of Japan’s main islands, in the East China Sea, is a Jurassic Park of longevity, with a higher percentage of centenarians (people who live to 100 years old) than anywhere else on Earth.
Hundreds of miles south of Japan’s main islands, in the East China Sea, is a Jurassic Park of longevity, with a higher percentage of centenarians (people who live to 100 years old) than anywhere else on Earth.