
TUFTS ‘HEALTH & NUTRITION LETTER’ (April 24, 2025):

TUFTS ‘HEALTH & NUTRITION LETTER’ (April 24, 2025):
Less than 7% of the U.S. adult population has good cardiometabolic health, a devastating health crisis requiring urgent action, according to research led by a team from the Friedman School of Nutrition Science and Policy at Tufts University in a pioneering perspective on cardiometabolic health trends and disparities published in the July 12 issue of the Journal of the American College of Cardiology. Their team also included researchers from Tufts Medical Center.
Researchers evaluated Americans across five components of health: levels of blood pressure, blood sugar, blood cholesterol, adiposity (overweight and obesity), and presence or absence of cardiovascular disease (heart attack, stroke, etc.). They found that only 6.8 percent of U.S. adults had optimal levels of all five components as of 2017-2018.

The majority of global COVID-19 deaths have been in countries where many people are obese, with coronavirus fatality rates 10 times higher in nations where at least 50% of adults are overweight, a global study found.
In this cross-sectional study of 5364 couples consisting of employees and spouses (or domestic partners) undergoing an annual employer-sponsored health assessment, 79% of the couples were in the nonideal category of a CV health score. This within-couple concordance of nonideal CV health scores was associated mostly with unhealthy diet and inadequate physical activity.

The study included 10 728 participants (5364 couples): 7% were African American, 11% Hispanic, 21% Asian, and 54% White (median [interquartile range] age, 50 [41-57] years for men and 47 [39-55] for women). For most couples, both members were in the ideal category or both were in a nonideal category.
Concordance ranged from 53% (95% CI, 52%-54%) for cholesterol to 95% (95% CI, 94%-95%) for diet. For the CV health score, in 79% (95% CI, 78%-80%) of couples both members were in a nonideal category, which was associated mainly with unhealthy diet (94% [95% CI, 93%-94%] of couples) and inadequate exercise (53% [95% CI, 52%-55%] of couples). However, in most couples, both members were in the ideal category for smoking status (60% [95% CI, 59%-61%] of couples) and glucose (56% [95% CI, 55%-58%]).
Except for total cholesterol, when 1 member of a couple was in the ideal category, the other member was likely also to be in the ideal category: the adjusted odds ratios for also being in the ideal category ranged from 1.3 (95% CI, 1.1-1.5; P ≤ .001) for blood pressure to 10.6 (95% CI, 7.4-15.3; P ≤ .001) for diet. Concordance differed by ethnicity, socioeconomic status, and geographic location.
From Phys.org/Univ. of Michigan (June 9, 2020):
 “On a high-sugar diet, we find that the fruit flies’ dopaminergic neurons are less active, because the high sugar intake decreases the intensity of the sweetness signal that comes from the mouth,” Dus said. “Animals use this feedback from dopamine to make predictions about how rewarding or filling a food will be. In the high-sugar diet flies, this process is broken—they get less dopamine neuron activation and so end up eating more than they need, which over time makes them gain weight.”
“On a high-sugar diet, we find that the fruit flies’ dopaminergic neurons are less active, because the high sugar intake decreases the intensity of the sweetness signal that comes from the mouth,” Dus said. “Animals use this feedback from dopamine to make predictions about how rewarding or filling a food will be. In the high-sugar diet flies, this process is broken—they get less dopamine neuron activation and so end up eating more than they need, which over time makes them gain weight.”
It is well known that consuming food and drink high in sugar is not great for us, but scientists are continuing to unravel the intricacies of how the sweet stuff drives negative health outcomes. The latest finding comes from researchers at the University of Michigan, who through studies in fruit flies have found that excess amounts of sugar can shut down crucial neural circuits linked to regulating satiety, possibly leading to overeating in humans.
From The Lancet Diabetes & Endocrinology (June 2020):
Our findings show that the intensive lifestyle intervention led to significant weight loss at 12 months, and was associated with diabetes remission in over 60% of participants and normoglycaemia in over 30% of participants. The provision of this lifestyle intervention could allow a large proportion of young individuals with early diabetes to achieve improvements in key cardiometabolic outcomes, with potential long-term benefits for health and wellbeing.

From Oxford University Press – OUP (May 1, 2020):
…ultra-processed foods are generally the foods available to nurses working nightshifts, firefighters returning to their department after a call, police officers  patrolling neighborhoods, or military soldiers during field-exercises. Thus, time-restricted eating removes the added stress of what to eat, and serves as a practical intervention conducive to the schedules of many people.
patrolling neighborhoods, or military soldiers during field-exercises. Thus, time-restricted eating removes the added stress of what to eat, and serves as a practical intervention conducive to the schedules of many people.
Time-restricted eating has been shown to lower circulating insulin, blood pressure, body fat and overall body weight, inflammation, and oxidative stress.
Time-restricted eating is a nutrition intervention which alternates between a period of fasting (12 – 16 hours) followed by a period of eating (8 – 12 hours). Unlike other diets, which focus on the caloric content of a meal or which foods you should eat, time-restricted eating focuses exclusively on when you eat by compressing and standardizing the feeding window each day. In turn, people following this type of eating pattern naturally enter a state of caloric deficit.

From a Diabetologia online study release (April 15, 2020):
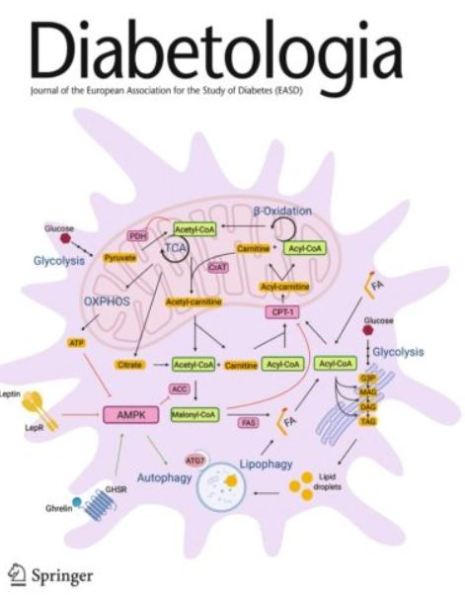 “Having normal body weight is crucial in the prevention of type 2 diabetes, regardless of genetic predisposition.”
“Having normal body weight is crucial in the prevention of type 2 diabetes, regardless of genetic predisposition.”
“The results suggest that type 2 diabetes prevention by weight management and healthy lifestyle is critical across all genetic risk groups.”
“Overall, the results indicate that a favorable lifestyle should be universally recommended in the prevention of type 2 diabetes, regardless of genetic predisposition, thus supporting current public health guidelines,”
We examined the joint association of genetic predisposition, obesity and unfavourable lifestyle with incident type 2 diabetes using a case-cohort study nested within the Diet, Cancer and Health cohort in Denmark. The study sample included 4729 individuals who developed type 2 diabetes during a median 14.7 years of follow-up, and a randomly selected cohort sample of 5402 individuals.
Obesity (BMI ≥ 30 kg/m2) and unfavourable lifestyle were associated with higher risk for incident type 2 diabetes regardless of genetic predisposition (p > 0.05 for GRS–obesity and GRS–lifestyle interaction). The effect of obesity on type 2 diabetes risk (HR 5.81 [95% CI 5.16, 6.55]) was high, whereas the effects of high genetic risk (HR 2.00 [95% CI 1.76, 2.27]) and unfavourable lifestyle (HR 1.18 [95% CI 1.06, 1.30]) were relatively modest.