From a The Lancet online article:
 As a consultant, I had profoundly failed to appreciate the experience of fatigue and apathy among patients. More than excessive tiredness, the fatigue was overwhelming, turning simple activities into insurmountable, exhausting challenges. It was frustrating and I fell into the trap of overexertion when I did have energy, thus exhausting myself and sabotaging the day’s recovery plan. Had staff not been so adept at encouraging me when I lacked energy and holding me back when I tried to overdo things, I would have squandered much valuable rehabilitation time.
As a consultant, I had profoundly failed to appreciate the experience of fatigue and apathy among patients. More than excessive tiredness, the fatigue was overwhelming, turning simple activities into insurmountable, exhausting challenges. It was frustrating and I fell into the trap of overexertion when I did have energy, thus exhausting myself and sabotaging the day’s recovery plan. Had staff not been so adept at encouraging me when I lacked energy and holding me back when I tried to overdo things, I would have squandered much valuable rehabilitation time.
I was a consultant in neurological rehabilitation for acquired brain injury when, at the age of 62 years, I had a stroke. Running for a train, I experienced pain in the right side of my head and mild weakness and sensory loss in my left limbs. I thought I’d had a stroke, but I was remarkably calm. It was late and my instinct was to get home, where I went to the study. In the morning, I found myself on the floor, half-blind, half-paralysed, and terrified.
.
Scans showed a large intracerebral haemorrhage in the area of the right basal ganglia. My symptoms could be explained by the damage to my brain—my medical world was in order, something to hold on to. I discussed my diagnosis and treatment with my colleagues during brief waking periods, grateful that they still saw the person I was before my stroke. Meanwhile, my wife was in the good hands of staff who treated her with sensitivity, giving her plain facts and support.
 Beyond the constant tossing and turning of a sleepless night, it might surprise you to know that insomnia is affecting a fair hunk of the Australian population. A recent study released by the Sleep Health Foundation found that 15 per cent of us suffer from chronic insomnia disorder, and very few people are choosing to access help.
Beyond the constant tossing and turning of a sleepless night, it might surprise you to know that insomnia is affecting a fair hunk of the Australian population. A recent study released by the Sleep Health Foundation found that 15 per cent of us suffer from chronic insomnia disorder, and very few people are choosing to access help.

 …a new study from the
…a new study from the  “A reduction in body weight of 12 percent is like getting a human from 200 pounds down to 176, which is a significant change,” said first author Md Nurunnabi, a former Postdoctoral Fellow at the Wyss Institute and SEAS who is now an Assistant Professor of Pharmaceutical Sciences at The University of Texas at El Paso. “Our goal is to translate this work into a product that can help people maintain a healthier weight, and this study marks the very beginning of that journey.”
“A reduction in body weight of 12 percent is like getting a human from 200 pounds down to 176, which is a significant change,” said first author Md Nurunnabi, a former Postdoctoral Fellow at the Wyss Institute and SEAS who is now an Assistant Professor of Pharmaceutical Sciences at The University of Texas at El Paso. “Our goal is to translate this work into a product that can help people maintain a healthier weight, and this study marks the very beginning of that journey.”
 The
The 


 They found that these physically active mice had fewer inflammatory cells (leukocytes) than sedentary mice, an effect they traced to diminished activity of hematopoietic stem and progenitor cells (HSPCs). The lower activity of HSPCs was due at least in part to exercise-induced reduction in the levels of leptin, a hormone produced by fat tissue that regulates cells within the hematopoietic bone marrow niche.
They found that these physically active mice had fewer inflammatory cells (leukocytes) than sedentary mice, an effect they traced to diminished activity of hematopoietic stem and progenitor cells (HSPCs). The lower activity of HSPCs was due at least in part to exercise-induced reduction in the levels of leptin, a hormone produced by fat tissue that regulates cells within the hematopoietic bone marrow niche.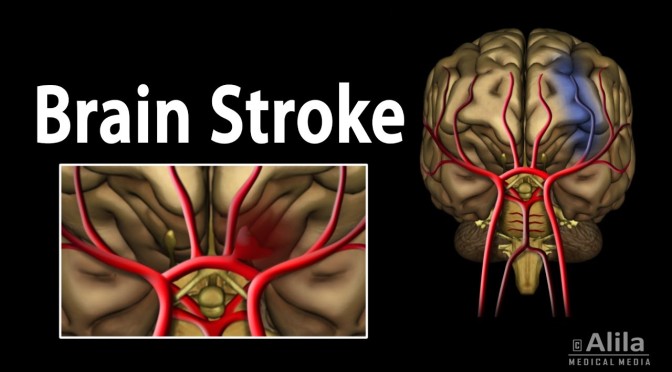
 As a consultant, I had profoundly failed to appreciate the experience of fatigue and apathy among patients. More than excessive tiredness, the fatigue was overwhelming, turning simple activities into insurmountable, exhausting challenges. It was frustrating and I fell into the trap of overexertion when I did have energy, thus exhausting myself and sabotaging the day’s recovery plan. Had staff not been so adept at encouraging me when I lacked energy and holding me back when I tried to overdo things, I would have squandered much valuable rehabilitation time.
As a consultant, I had profoundly failed to appreciate the experience of fatigue and apathy among patients. More than excessive tiredness, the fatigue was overwhelming, turning simple activities into insurmountable, exhausting challenges. It was frustrating and I fell into the trap of overexertion when I did have energy, thus exhausting myself and sabotaging the day’s recovery plan. Had staff not been so adept at encouraging me when I lacked energy and holding me back when I tried to overdo things, I would have squandered much valuable rehabilitation time. 
 There can be few applications of digital technology more worthwhile than saving lives, but integrating digital technology into healthcare systems is uniquely complex. This episode provides an introduction to some of the challenges that healthcare providers face in their pursuit of digital innovation, and explores some of the paths forward.
There can be few applications of digital technology more worthwhile than saving lives, but integrating digital technology into healthcare systems is uniquely complex. This episode provides an introduction to some of the challenges that healthcare providers face in their pursuit of digital innovation, and explores some of the paths forward. The riders who had pedaled on an empty stomach, however, had incinerated about twice as much fat during each ride as the men who consumed the shake first. The riders all had burned about the same number of calories while pedaling, but more of those calories came from fat when the men did not eat first.
The riders who had pedaled on an empty stomach, however, had incinerated about twice as much fat during each ride as the men who consumed the shake first. The riders all had burned about the same number of calories while pedaling, but more of those calories came from fat when the men did not eat first.
 Medicare negotiation of prescription-drug prices would bring U.S. government policies in line with those of other high-income countries, and the idea is popular with both the public and policy analysts. But it would represent a sea change for pharmaceutical firms, which will maintain that any threat to their pricing power will slow innovation.
Medicare negotiation of prescription-drug prices would bring U.S. government policies in line with those of other high-income countries, and the idea is popular with both the public and policy analysts. But it would represent a sea change for pharmaceutical firms, which will maintain that any threat to their pricing power will slow innovation.