
Infographic: Brain Health, Strokes & Healthy Aging


From 2019 to 2020, there was a substantial increase in the proportion of older adults who reported that their health care providers offered telehealth visits. In May 2019, 14% of older adults said that their health care providers offered telehealth visits, compared to 62% in June 2020.
Similarly, the percentage of older adults who had ever participated in a telehealth visit rose sharply from 4% in May 2019 to 30% in June 2020. Of those surveyed in 2020, 6% reported having a telehealth visit prior to March 2020, while 26% reported having a telehealth visit in the period from March to June 2020.

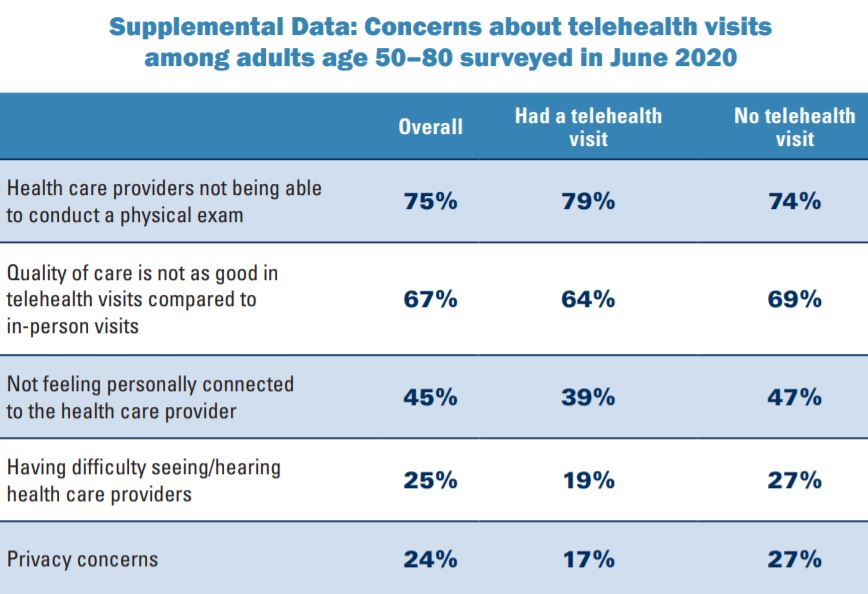
Over the past year, some concerns about telehealth visits decreased among adults age 50–80 whether or not they had a telehealth visit. Older adults’ concerns about privacy in telehealth visits decreased from 49% in May 2019 to 24% in June 2020, and concerns about having difficulty seeing or hearing health care providers in telehealth visits decreased from 39% in May 2019 to 25% in June 2020. Concerns about not feeling personally connected to the health care provider decreased slightly (49% to 45%).

HARVARD MAGAZINE (SEPT – OCT 2020): From the book EXERCISED: Why Something We Never Evolved to Do Is Healthy and Rewarding by Daniel E. Lieberman, to be published on September 8, 2020 by Pantheon Books:

In order to elucidate the links between exercise and aging, I propose a corollary to the Grandmother Hypothesis, which I call the Active Grandparent Hypothesis. According to this idea, human longevity was not only selected for but was also made possible by having to work hard during old age to help as many children, grandchildren, and other younger relatives as possible survive and thrive. That is, while there may have been selection for genes (as yet unidentified) that help humans live past the age of 50, there was also selection for genes that repair and maintain our bodies when we are physically active.
Daniel E. Lieberman is a paleoanthropologist at Harvard University, where he is the Edwin M Lerner II Professor of Biological Sciences, and Professor in the Department of Human Evolutionary Biology. He is best known for his research on the evolution of the human head and the evolution of the human body.
‘Journal of Neurology, Neurosurgery & Psychiatry” (July 10, 2020):
 We tested the hypothesis that apathy, but not depression, is associated with dementia in patients with SVD. We found that higher baseline apathy, as well as increasing apathy over time, were associated with an increased dementia risk. In contrast, neither baseline depression or change in depression was associated with dementia. The relationship between apathy and dementia remained after controlling for other well-established risk factors including age, education and cognition. Finally, adding apathy to models predicting dementia improved model fit. These results suggest that apathy may be a prodromal symptom of dementia in patients with SVD.
We tested the hypothesis that apathy, but not depression, is associated with dementia in patients with SVD. We found that higher baseline apathy, as well as increasing apathy over time, were associated with an increased dementia risk. In contrast, neither baseline depression or change in depression was associated with dementia. The relationship between apathy and dementia remained after controlling for other well-established risk factors including age, education and cognition. Finally, adding apathy to models predicting dementia improved model fit. These results suggest that apathy may be a prodromal symptom of dementia in patients with SVD.
Cerebral small vessel disease (SVD) is the leading vascular cause of dementia and plays a major role in cognitive decline and mortality.1 2 SVD affects the small vessels of the brain, leading to damage in the subcortical grey and white matter.1 The resulting clinical presentation includes cognitive and neuropsychiatric symptoms.1
Apathy is a reduction in goal-directed behaviour, which is a common neuropsychiatric symptom in SVD.3 Importantly, apathy is dissociable from depression,3 4 another symptom in SVD for which low mood is a predominant manifestation.5 Although there is some symptomatic overlap between the two,6 research using diffusion imaging reported that apathy, but not depression, was associated with white matter network damage in SVD.3 Many of the white matter pathways underlying apathy overlap with those related to cognitive impairment, and accordingly apathy, rather than depression, has been associated with cognitive deficits in SVD.7 These results suggest that apathy and cognitive impairment are symptomatic of prodromal dementia in SVD.
Dr. Aimee Kao discusses key behaviors known to protect brain health. Dr. Kao looks at population trends and wonders if they tell a complete story. Watch full lecture here:
From AMA.org (June 12, 2020):
 “There’s an aging population, and there’s a lot of skin out there,” said Dr. Isaacs. “One in five people in the country develop skin cancer, but there is a plethora of benign skin conditions that also require the expertise of the dermatologist. So, you have increasing demand and a limited supply of dermatologists.”
“There’s an aging population, and there’s a lot of skin out there,” said Dr. Isaacs. “One in five people in the country develop skin cancer, but there is a plethora of benign skin conditions that also require the expertise of the dermatologist. So, you have increasing demand and a limited supply of dermatologists.”
A basic example of how the TPMG teledermatology program works involves a patient who is concerned about a suspicious lesion or mole on their body. The patient can take a picture of the location in question and send it to their primary care physician for review. The physician can request the patient come in for a more thorough evaluation, or if the physician determines that a dermatologist should be involved, they can send the photo to an on-call dermatologist to review.
If the patient does an in-person evaluation, the physician can also take a higher-quality image and forward that to a dermatologist. The dermatologist can then decide whether there is a problem, if a prescription is needed, or if there should be an in-person evaluation and potential biopsy.
A study in the Journal of the American Academy of Dermatology in 2019 found that when TPMG dermatologists had the chance to look at well-photographed skin lesions, they were able to identify nearly 10% more cancers with almost 40% fewer referrals to the dermatology department.
We observed that increased adherence to the MedDiet modulates specific components of the gut microbiota that were associated with a reduction in risk of frailty, improved cognitive function and reduced inflammatory status.
Dr Philip Smith, Digital and Education Editor of Gut and Consultant Gastroenterologist at the Royal Liverpool Hospital interviews Professor Paul O’Toole; who is Professor of Microbial Genomics, Head of School of Microbiology and Principal Investigator in APC Microbiome Ireland, an SFI funded centre at University College Cork, Ireland, on “Mediterranean diet intervention alters the gut microbiome in older people reducing frailty and improving health status: the NU-AGE 1-year dietary intervention across 5 European countries” published in paper copy in Gut in July 2020.
From the American Journal of Clinical Nutrition (April 22, 2020):
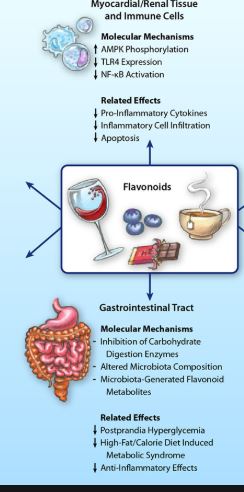 Our findings imply that higher long-term dietary intakes of flavonoids are associated with lower risks of ADRD and AD in US adults.
Our findings imply that higher long-term dietary intakes of flavonoids are associated with lower risks of ADRD and AD in US adults.Our findings provide new evidence that diets higher in flavonols, anthocyanins, and flavonoid polymers are associated with a lower risk of developing ADRD. These associations were sustained after accounting for a variety of potential confounders including key nutrients related to ADRD risk and overall diet quality. Similar findings were seen with AD risk for flavonols and anthocyanins but the association with flavonoid polymers was no longer statistically significant.
Along with improvements in healthcare and medical technology, the aging of the baby boom generation will result in an unprecedented rise in the number of older Americans (1, 2). Currently, there are >50 million Americans aged ≥65 y, and that is projected to more than double by 2060 (3). A consequence of this increase in older adults is the escalation of age-related diseases (4, 5). Alzheimer disease (AD) and related dementias (ADRD), a group of symptoms in which there is progressive deterioration in cognitive function severe enough to interfere with a person’s daily living activities, are regarded as among the most significant public health challenges largely affecting adults aged >65 y (6). AD is the most common form of dementia, making up ∼60–80% of dementia cases. Currently, 5.8 million Americans are living with AD, and by 2050 that is projected to escalate to 14 million (7).
 Health journalist Judy Foreman talks about her new book Exercise Is Medicine: How Physical Activity Boosts Health and Slows Aging
Health journalist Judy Foreman talks about her new book Exercise Is Medicine: How Physical Activity Boosts Health and Slows Aging This is Scientific American’s Science Talk, posted on April 24th, 2020. I’m Steve Mirsky. And under our current, often locked-down situation, it’s still really important to try to get some exercise. Judy Foreman is the author of the new book Exercise is Medicine: How Physical Activity Boosts Health and Slows Aging. She’s a former nationally syndicated health columnist for the Boston Globe, LA times, Baltimore Sun and other places, and an author for the Oxford University Press.
This is Scientific American’s Science Talk, posted on April 24th, 2020. I’m Steve Mirsky. And under our current, often locked-down situation, it’s still really important to try to get some exercise. Judy Foreman is the author of the new book Exercise is Medicine: How Physical Activity Boosts Health and Slows Aging. She’s a former nationally syndicated health columnist for the Boston Globe, LA times, Baltimore Sun and other places, and an author for the Oxford University Press.
She graduated Phi Beta Kappa from Wellesley College and has a Master’s from the Harvard Graduate School of Education. She was a Lecturer on Medicine at Harvard Medical School, a Fellow in Medical Ethics at Harvard Medical School and a Knight Science Journalism Fellow at the Massachusetts Institute of Technology. She spent six months as a guest reporter for The Times of London. She was also a Senior Fellow at the Schuster Institute for Investigative Journalism at Brandeis University. She was also host of a live, weekly call-in radio show on Healthtalk.com.
Judy has won more than 50 journalism awards, including a 1998 George Foster Peabody award for co-writing a video documentary about a young woman dying of breast cancer and the 2015 Science in Society award from the National Association of Science Writers.
https://www.youtube.com/watch?v=DupyoYqtxnc
Presented by Sarah Dulaney, RN, CNS, a nurse at the UCSF Memory and Aging Center, and Helen Medsger, a family caregiver and LBD support group leader, as part of the Lewy Body Dementia Caregiver Webinar Series supported by the UCSF Memory and Aging Center and the Administration for Community Living.