From a BMJ online article:
We derived a healthy lifestyle score based on information on five lifestyle factors—diet, smoking, physical activity, alcohol consumption, and body mass index (BMI).
 Our findings suggest that promotion of a healthy lifestyle would help to reduce the healthcare burdens through lowering the risk of developing multiple chronic diseases, including cancer, cardiovascular disease, and diabetes, and extending disease-free life expectancy. Public policies for improving food and the physical environment conducive to adopting a healthy diet and lifestyle, as well as relevant policies and regulations (for example, smoking ban in public places or trans-fat restrictions), are critical to improving life expectancy, especially life expectancy free of major chronic diseases.
Our findings suggest that promotion of a healthy lifestyle would help to reduce the healthcare burdens through lowering the risk of developing multiple chronic diseases, including cancer, cardiovascular disease, and diabetes, and extending disease-free life expectancy. Public policies for improving food and the physical environment conducive to adopting a healthy diet and lifestyle, as well as relevant policies and regulations (for example, smoking ban in public places or trans-fat restrictions), are critical to improving life expectancy, especially life expectancy free of major chronic diseases.
The average life expectancy in the world has increased substantially in the past few decades. The aging of the population has led to a high prevalence of chronic diseases such as diabetes, cardiovascular disease, and cancer. Although people live longer, older individuals often live with disabilities and chronic diseases. People with chronic diseases including cancer, cardiovascular disease, and diabetes have a shorter life expectancy than do their peers without these chronic conditions. Estimates of the loss in life years due to these chronic conditions range from 7.5 to 20 years, depending on the methods used and the characteristics of the study population.
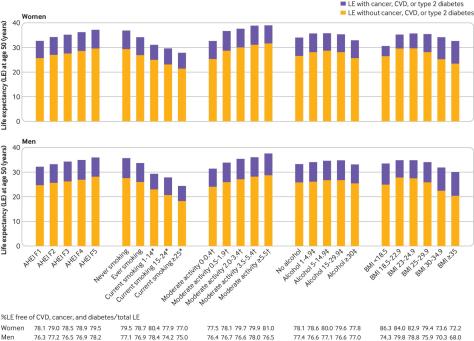
Modifiable lifestyle factors including smoking, physical activity, alcohol intake, body weight, and diet quality affect both total life expectancy and incidence of chronic diseases. Studies have shown that smoking, inactivity, poor diet quality, and heavy alcohol consumption contribute up to 60% of premature deaths and 7.4-17.9 years’ loss in life expectancy. Nevertheless, little research has looked at how a combination of multiple lifestyle factors may relate to life expectancy free from the major diseases of diabetes, cardiovascular disease, and cancer.





 In our own study of more than 7,000 middle-aged to older adults in the U.K., published in 2019 in Brain Imaging and Behavior, we demonstrated that people who spent more time engaged in moderate to vigorous physical activity had larger hippocampal volumes. Although it is not yet possible to say whether these effects in humans are related to neurogenesis or other forms of brain plasticity, such as increasing connections among existing neurons, together the results clearly indicate that exercise can benefit the brain’s hippocampus and its cognitive functions.
In our own study of more than 7,000 middle-aged to older adults in the U.K., published in 2019 in Brain Imaging and Behavior, we demonstrated that people who spent more time engaged in moderate to vigorous physical activity had larger hippocampal volumes. Although it is not yet possible to say whether these effects in humans are related to neurogenesis or other forms of brain plasticity, such as increasing connections among existing neurons, together the results clearly indicate that exercise can benefit the brain’s hippocampus and its cognitive functions.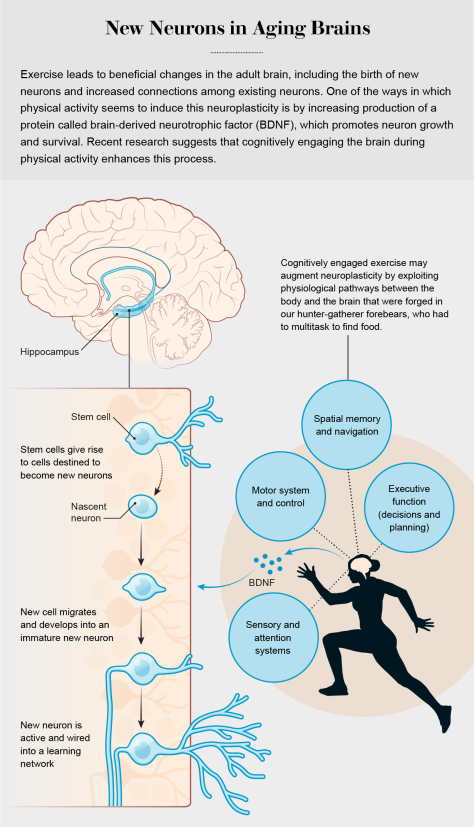


 …primary care providers (general practice, paediatrics, and internal medicine) performed the best, giving a considerably lower percentage of antibiotic prescriptions without a documented indication (12%) than other specialists such as gynaecologists and urologists, who commonly prescribed antibiotics (24%), as well as those in all other specialties (29%).
…primary care providers (general practice, paediatrics, and internal medicine) performed the best, giving a considerably lower percentage of antibiotic prescriptions without a documented indication (12%) than other specialists such as gynaecologists and urologists, who commonly prescribed antibiotics (24%), as well as those in all other specialties (29%).
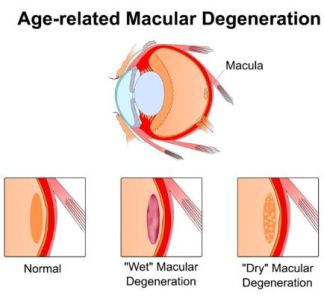 “Our work provides additional evidence that that diet matters,” Millen added. “From a public health standpoint, we can tell people that if you have early AMD, it is likely in your best interest to limit your intake of processed meat, fried food, refined grains, and high-fat dairy to preserve your vision over time.”
“Our work provides additional evidence that that diet matters,” Millen added. “From a public health standpoint, we can tell people that if you have early AMD, it is likely in your best interest to limit your intake of processed meat, fried food, refined grains, and high-fat dairy to preserve your vision over time.”
 This cohort study included 146 152 individuals from the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial and found that aspirin use 3 or more times per week was associated with reduced risk of all-cause, cancer, gastrointestinal cancer, and colorectal cancer mortality.
This cohort study included 146 152 individuals from the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial and found that aspirin use 3 or more times per week was associated with reduced risk of all-cause, cancer, gastrointestinal cancer, and colorectal cancer mortality.