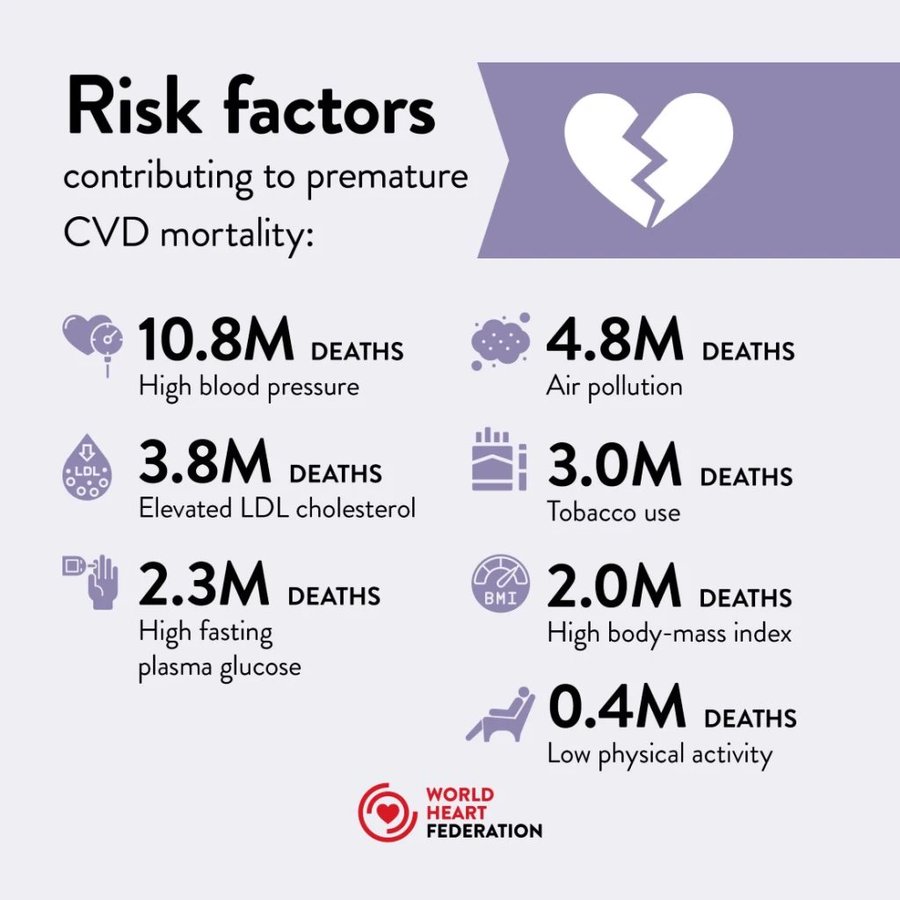
Globally, more people die from cardiovascular disease every year than from any other cause.

DOWNLOAD Report
Globally, more people die from cardiovascular disease every year than from any other cause.

DOWNLOAD Report

Published online by Cambridge University Press: 22 March 2021
As we age, there are characteristic changes in our thinking, reasoning and memory skills (referred to as cognitive ageing). However, variation between people in the timing and degree of change experienced suggests that a range of factors determine individual cognitive ageing trajectories. This narrative review considers some of the lifestyle factors that might promote (or harm) cognitive health. The focus on lifestyle factors is because these are potentially modifiable by individuals or may be the targets of behavioural or societal interventions. To support that, the review briefly considers people’s beliefs and attitudes about cognitive ageing; the nature and timing of cognitive changes across the lifespan; and the genetic contributions to cognitive ability level and change. In introducing potentially modifiable determinants, a framing that draws evidence derived from epidemiological studies of dementia is provided, before an overview of lifestyle and behavioural predictors of cognitive health, including education and occupation, diet and activity.
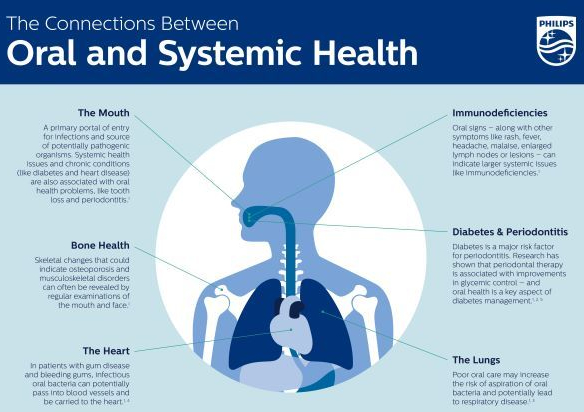
People today want to be more in control of their own health and are more attuned to getting the support and information they need online, from apps, and from connected products. Yet there are gaps in both their knowledge and daily commitment to good oral hygiene, and they need help along the way. Depending on lifestage, patient’s oral health concerns can evolve from plaque removal and aesthetics to larger concerns around gum health and disease. Too often, by the time they begin thinking about gum health, it’s too late. Multiple studies have revealed linkages between periodontal diseases and certain systemic diseases, such as diabetes, heart disease and kidney disease [4][5][6].
Prevention is key. Along with professional deep cleaning, good daily brushing and interdental cleaning are critical. It’s also important for patients to have regular conversations with their dentist about oral health issues and the linkage to their overall health.
There are lots of things you can do to prevent heart disease! The key is to live a healthy lifestyle and see your doctor for regular checkups.
To learn more about heart disease risk factors, please visit https://cle.clinic/3r3iKQh
In this cross-sectional study of 5364 couples consisting of employees and spouses (or domestic partners) undergoing an annual employer-sponsored health assessment, 79% of the couples were in the nonideal category of a CV health score. This within-couple concordance of nonideal CV health scores was associated mostly with unhealthy diet and inadequate physical activity.

The study included 10 728 participants (5364 couples): 7% were African American, 11% Hispanic, 21% Asian, and 54% White (median [interquartile range] age, 50 [41-57] years for men and 47 [39-55] for women). For most couples, both members were in the ideal category or both were in a nonideal category.
Concordance ranged from 53% (95% CI, 52%-54%) for cholesterol to 95% (95% CI, 94%-95%) for diet. For the CV health score, in 79% (95% CI, 78%-80%) of couples both members were in a nonideal category, which was associated mainly with unhealthy diet (94% [95% CI, 93%-94%] of couples) and inadequate exercise (53% [95% CI, 52%-55%] of couples). However, in most couples, both members were in the ideal category for smoking status (60% [95% CI, 59%-61%] of couples) and glucose (56% [95% CI, 55%-58%]).
Except for total cholesterol, when 1 member of a couple was in the ideal category, the other member was likely also to be in the ideal category: the adjusted odds ratios for also being in the ideal category ranged from 1.3 (95% CI, 1.1-1.5; P ≤ .001) for blood pressure to 10.6 (95% CI, 7.4-15.3; P ≤ .001) for diet. Concordance differed by ethnicity, socioeconomic status, and geographic location.
The number of older people, including those living with dementia, is rising, as younger age mortality declines. However, the age-specific incidence of dementia has fallen in many countries, probably because of improvements in education, nutrition, health care, and lifestyle changes.
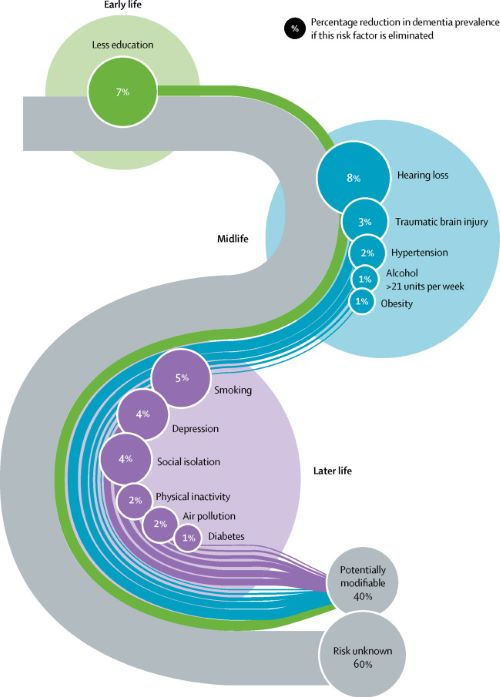
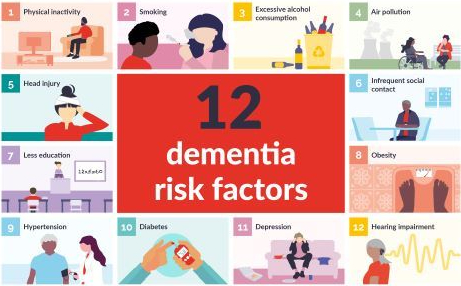
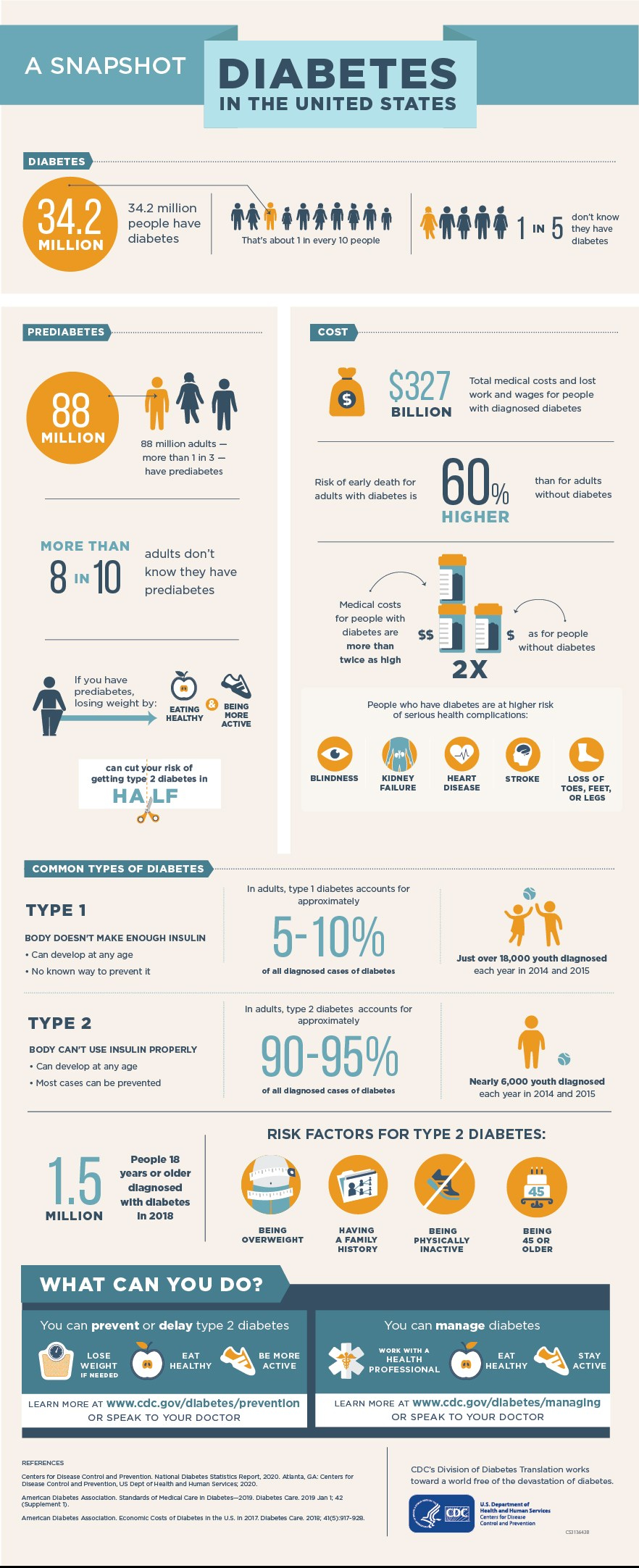
Overall, a growing body of evidence supports the nine potentially modifiable risk factors for dementia modelled by the 2017 Lancet Commission on dementia prevention, intervention, and care: less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, and low social contact.
We now add three more risk factors for dementia with newer, convincing evidence. These factors are excessive alcohol consumption, traumatic brain injury, and air pollution. We have completed new reviews and meta-analyses and incorporated these into an updated 12 risk factor life-course model of dementia prevention. Together the 12 modifiable risk factors account for around 40% of worldwide dementias, which consequently could theoretically be prevented or delayed.
The potential for prevention is high and might be higher in low-income and middle-income countries (LMIC) where more dementias occur. Our new life-course model and evidence synthesis has paramount worldwide policy implications. It is never too early and never too late in the life course for dementia prevention. Early-life (younger than 45 years) risks, such as less education, affect cognitive reserve; midlife (45–65 years), and later-life (older than 65 years) risk factors influence reserve and triggering of neuropathological developments.
Culture, poverty, and inequality are key drivers of the need for change. Individuals who are most deprived need these changes the most and will derive the highest benefit.
Diabetologia (Sept 8, 2020) – Insomnia with objective short sleep duration has been associated with an increased risk of type 2 diabetes in observational studies [27, 28]. The present MR study found strong and suggestive evidence of a causal association of insomnia and short sleep duration, respectively, with increased risk of type 2 diabetes.

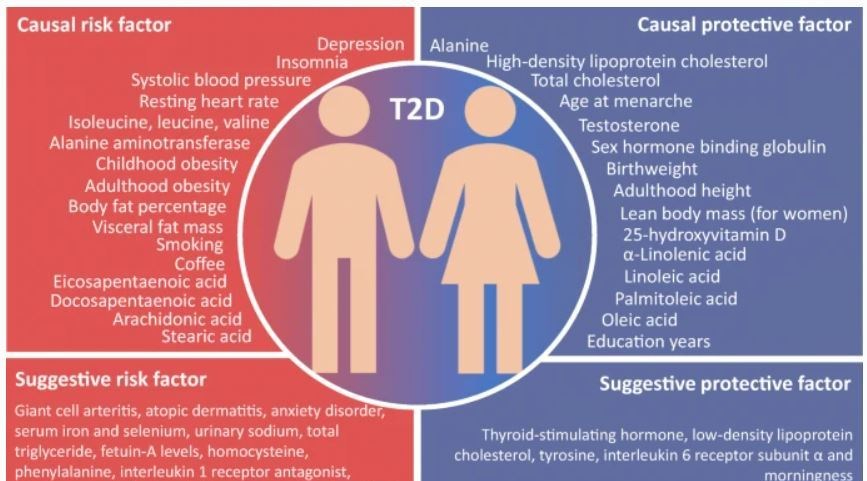
The present study verified several previously reported risk factors and identified novel potential risk factors for type 2 diabetes. Prevention strategies for type 2 diabetes should be considered from multiple perspectives on obesity, mental health, sleep quality, education level, birthweight and smoking.
From a BMJ Open Heart online study (March 8, 2020):
 Overall, the evidence in the literature suggests that spirulina improves several well-established CVD risk factors including hyperlipidaemia and seems to provide benefits around weight loss.
Overall, the evidence in the literature suggests that spirulina improves several well-established CVD risk factors including hyperlipidaemia and seems to provide benefits around weight loss.
Although caloric restriction and exercise are the mainstay treatments for obesity, spirulina has shown significant benefits in aiding weight loss. The phycocyanin in spirulina contains a light-harvesting chromophore called phycocyanobilin, which is capable of inhibiting nicotinamide adenine dinucleotide phosphate hydrogen (NADPH) oxidase, a significant source of oxidative stress in adipocytes playing a key role in inducing insulin resistance and shifting adipokine and cytokine production in hypertrophied adipocytes. Thus, by suppressing adipocyte oxidative stress, spirulina may lead to systemic anti-inflammatory and insulin-sensitising effects.
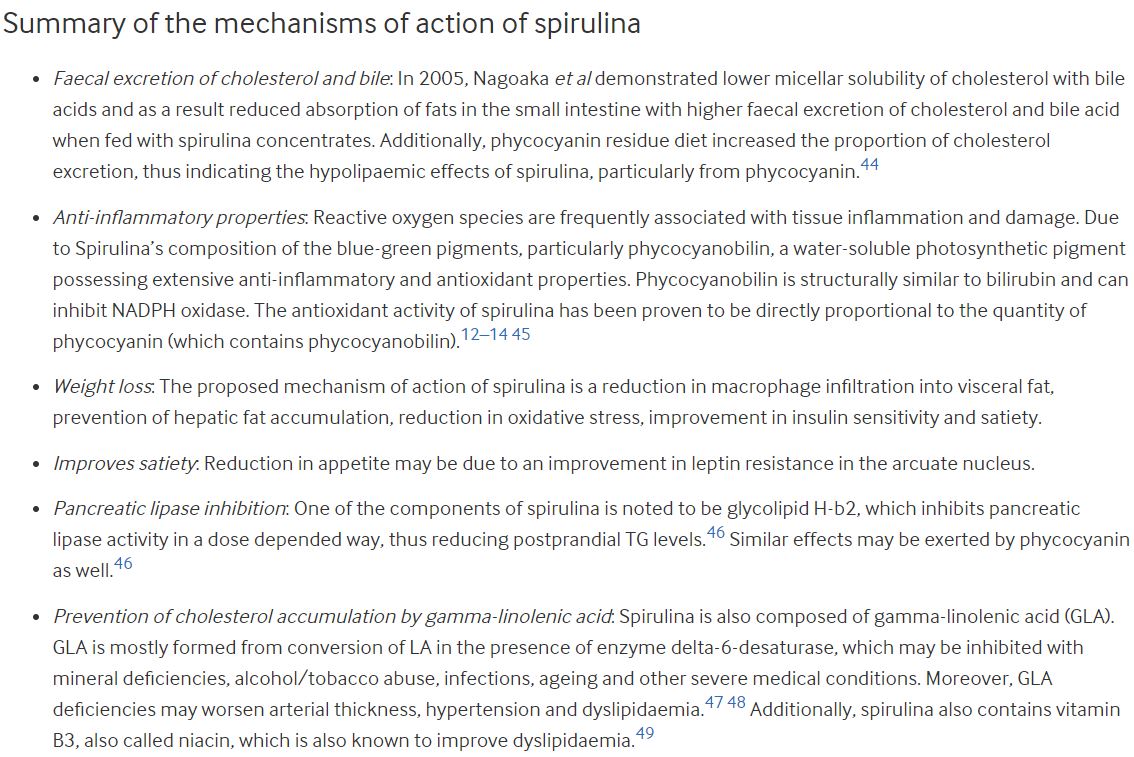
Spirulina is both a salt and fresh water blue-green algae, which is being increasingly studied recently. Spirulina was initially classified under the plant kingdom due to its rich plant pigments and its ability to photosynthesize, but was later placed into bacterial kingdom (cyanobacteria) due to its genetic, physiological and biochemical makeup. Spirulina grows naturally in high salt alkaline water reservoirs in subtropical and tropical areas of America, Mexico, Asia and Central Africa.