For many people, depression turns out to be one of the most disabling illnesses that we have in society. Despite the treatments that we have available, many people are not responding that well. It’s a disorder that can be very disabling in society. It’s also a disorder that has medical consequences. By understand the neurobiology of depression we hope to be able more to find the right treatment for the patient suffering from this disease. The current standard of care for the treatment of depression is based on what we call the monoamine deficiency hypothesis. Essentially, presuming that one of three neurotransmitters in the brain is deficient or underactive. But the reality is, there are more than 100 neurotransmitters in the brain. And billions of connections between neurons. So we know that that’s a limited hypothesis. Neurotransmitters can be thought of as the chemical messengers within the brain, it’s what helps one cell in the brain communicate with another, to pass that message along from one brain region to another. For decades, we thought that the primary pathology, the primary cause of depression was some abnormality in these neurotransmitters, specifically serotonin or norepinephrine. However, norepinephrine and serotonin did not seem to be able to account for this cause, or to cause the symptoms of depression in people who had major depression. Instead, the chemical messengers between the nerve cells in the higher centers of the brain, which include glutamate and GABA, were possibilities as alternative causes for the symptoms of depression. When you’re exposed to severe and chronic stress like people experience when they have depression, you lose some of the connections between the nerve cells. The communication in these circuits becomes inefficient and noisy, we think that the loss of these synaptic connections contributes to the biology of depression. There are clear differences between a healthy brain and a depressed brain. And the exciting thing is, when you treat that depression effectively, the brain goes back to looking like a healthy brain, both at the cellular level and at a global scale. It’s critical to understand the neurobiology of depression and how the brain plays a role in that for two main reasons. One, it helps us understand how the disease develops and progresses, and we can start to target treatments based on that. We are in a new era of psychiatry. This is a paradigm shift, away from a model of monoaminergic deficiency to a fuller understanding of the brain as a complex neurochemical organ. All of the research is driven by the imperative to alleviate human suffering. Depression is one of the most substantial contributors to human suffering. The opportunity to make even a tiny dent in that is an incredible opportunity.SHOW LESS
Tag Archives: Mental Health
Morning News Podcast: Facebook Upholds Trump Ban, Juvenile Offenders
The social-media giant’s external-review body upheld a ban on former president Donald Trump—for now. We ask how a narrow ruling reflects on far broader questions of free speech and regulation.
America’s young offenders are often handed long sentences and face disproportionate harms; we examine reforms that are slowly taking hold. And the Broadway mental-health musical that is a surprise hit in China.
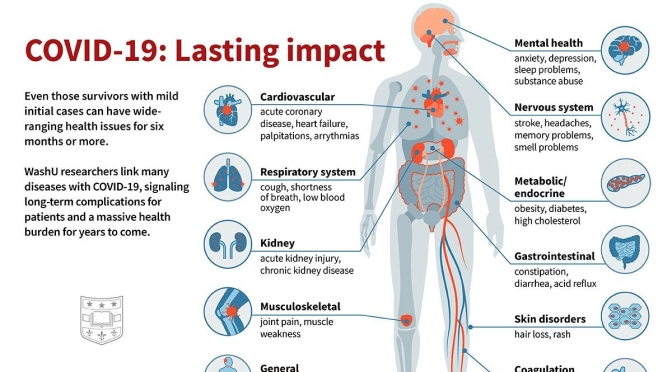
Covid-19 Infographic: Mental Health Among Older Adults Age 50-80
Infographic: Lasting Impacts Of Covid-19

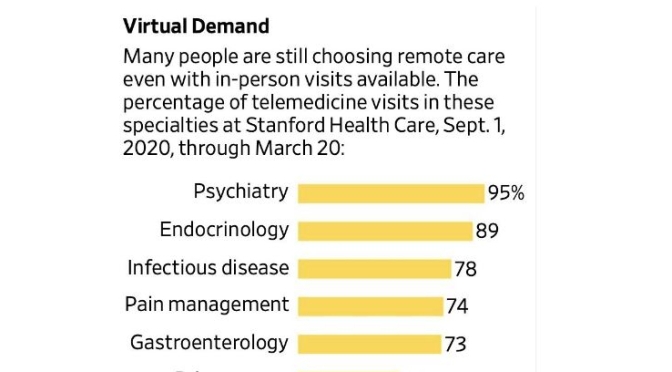
Telemedicine Survey: ‘High Demand’ Continues For Virtual Medical Visits
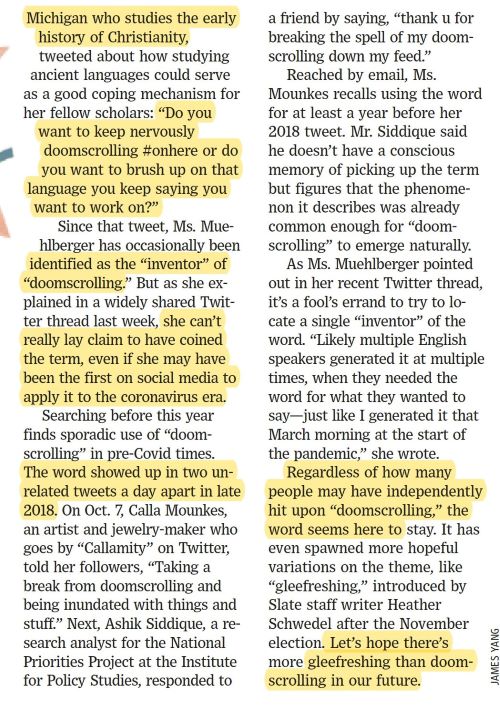
Social Media & Health: ‘Doomscrolling’ Your Way To Despair & Depression
Morning News Podcast: Supreme Court Choice, Mental Health Care In CA

NPR News Now reports: President Trump expected to announce Amy Coney Barrett as choice for Supreme Court, mental health care in California, Oregon wildfires and other top news.
Health: “Chasing The Sun – How Light And Dark Shape Our Bodies And Minds”
Human biology is tuned to a 24-hour light-dark cycle but modern lifestyles are disrupting it with unhealthy consequences, says Linda Geddes
Reading Lists: “The Best Neuroscience Books Of 2019” (TheScientist)

Bury your nose in tales of neurosyphilis, gender identity, the medical mysteries of sleep disorders, and more. JAMES DOLBOW

The Nocturnal Brain: Nightmares, Neuroscience and the Secret World of Sleep
Inspired by the legendary book The Man Who Mistook His Wife for a Hat by the late Oliver Sacks, neurologist and sleep scientist Guy Leschziner tells the curious true stories of his patients, their fascinating sleep disorders, and the neuroscience behind each. Also like the works of Sacks, The Nocturnal Brain is written with considerable introspection and wonder about each patient’s case, taking you on a journey from the first patient encounter, to diagnosis, and through treatment. The unusual and often bizarre cases will keep you intrigued and immersed, and make this unique book one you will find yourself looking forward to making time to read.
 How The Brain Lost Its Mind: Sex, Hysteria, and the Riddle of Mental Health
How The Brain Lost Its Mind: Sex, Hysteria, and the Riddle of Mental Health
In this mindful reflection on American and European pasts, authors Allan H. Ropper and Brian Burrell, also the writers of Reaching Down the Rabbit Hole, address our modern concept of mental illness by reviewing the interesting true story of the syphilis epidemic of the 19th century. This little known and fascinating history of neurosyphilis—how it was handled by society and medicine and how it shaped today’s understanding of mental illness—helps address not only why many stigmas exist, but why so many have persisted. This book will take you on an incredible journey through the puzzling diagnosis, eclectic treatments, and lasting social effects of the neurosyphilis epidemic of the 1800s, as well as offer important insight into the difference between diseases of the brain and the mind. This book is perfect for any scientist, psychologist, or historian with even the smallest interest in medical history or mental health theory.
 Compassionomics: The Revolutionary Scientific Evidence that Caring Makes a Difference
Compassionomics: The Revolutionary Scientific Evidence that Caring Makes a Difference
It is no secret that today’s medical atmosphere scarsely resembles anything similar to that of 50 years ago. Many have argued that this is in large part due to a lack of compassion in the modern medical system. If this is the case, where have we gone wrong, and is there scientific evidence to support that compassion is even beneficial to healthcare, personal relationships, and professional lives? These questions are raised and explored by authors Stephen Trzeciak and Anthony Mazzarelli through the telling of true stories of medical providers and patients that help demonstrate the incredible effect of the human connection. Coupled perfectly with these gripping stories are easily readable summaries of decades of research studying the effects of compassion as well as its implications in our lives. Addressing topics from healthcare cost to provider burnout, from caring for others to caring for ourselves, this evidence-based analysis of the importance of compassion is a must-read for anyone interested in the social science and psychology of the care we give in all settings of our lives.
To read more: https://www.the-scientist.com/news-opinion/opinion–the-best-neuroscience-books-of-2019-66863
New Mental Health Books: “The Great Pretender” By Susannah Cahalan Looks At “Madness” In Society
Psychiatry, as a distinct branch of medicine, has come far in its short life span. (The term psychiatrist is less than 150 years old.) The field has rejected the famously horrific practices of the recent past—the lobotomies, forced sterilizations, human warehousing. Today’s psychiatric practitioners boast a varied arsenal of effective drugs and have largely dropped the unscientific trappings of psychoanalytic psychobabble, the “schizophrenogenic mothers” of yesteryear who had been thought to have somehow triggered insanity in their unwitting offspring. Two decades into the 21st century, psychiatry now views severe mental illnesses as legitimate brain diseases. Despite all these advancements, however, the field still relies solely on self-reported symptoms and observable signs for diagnosis. Though the American Psychiatry Association reassures us that psychiatrists are uniquely qualified to “assess both the mental and physical aspects of psychological problems,” they are, like all of medicine, limited by the tools at hand. There are not, as of this writing, any consistent objective measures that can render a definitive psychiatric diagnosis.