From a
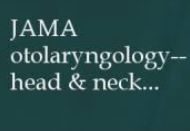 Cell phone–related injuries to the head and neck have increased steeply over the recent 20-year period, with many cases resulting from distraction. Although the disposition of most cases is simple, some injuries bear a risk of long-term complications. Many of these injuries occurred among those aged 13 to 29 years and were associated with common activities, such as texting while walking. These findings suggest a need for patient education about injury prevention and the dangers of activity while using these devices.
Cell phone–related injuries to the head and neck have increased steeply over the recent 20-year period, with many cases resulting from distraction. Although the disposition of most cases is simple, some injuries bear a risk of long-term complications. Many of these injuries occurred among those aged 13 to 29 years and were associated with common activities, such as texting while walking. These findings suggest a need for patient education about injury prevention and the dangers of activity while using these devices.
Since their invention, cell phones have played a major role in the daily lives of American adults. Approximately 96% of Americans own a cell phone, provoking interest in their role in causing injury. Given that head and neck traumas make up approximately 5% of emergency department (ED) visits in the United States, cell phone use in relation to such injuries could be of public health concern, in particular because of the psychological and financial burdens such injuries may entail. In addition, knowledge of the mechanism of injury is vital for patient risk stratification and trauma management,and understanding the mechanisms of common cell phone–related injuries can aid health care professionals in assessing patient needs. Health care professionals and public safety officials also must be aware of the epidemiologic nature of such injuries in order to provide adequate counseling and give input for legislation to protect the population.



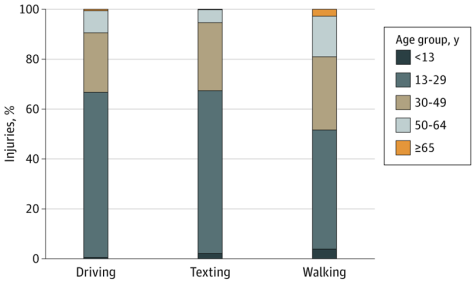
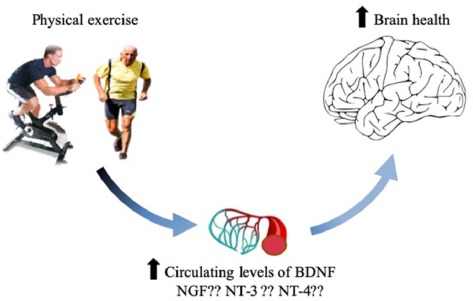
 Our findings suggest that promotion of a healthy lifestyle would help to reduce the healthcare burdens through lowering the risk of developing multiple chronic diseases, including cancer, cardiovascular disease, and diabetes, and extending disease-free life expectancy. Public policies for improving food and the physical environment conducive to adopting a healthy diet and lifestyle, as well as relevant policies and regulations (for example, smoking ban in public places or trans-fat restrictions), are critical to improving life expectancy, especially life expectancy free of major chronic diseases.
Our findings suggest that promotion of a healthy lifestyle would help to reduce the healthcare burdens through lowering the risk of developing multiple chronic diseases, including cancer, cardiovascular disease, and diabetes, and extending disease-free life expectancy. Public policies for improving food and the physical environment conducive to adopting a healthy diet and lifestyle, as well as relevant policies and regulations (for example, smoking ban in public places or trans-fat restrictions), are critical to improving life expectancy, especially life expectancy free of major chronic diseases.

 “This is an entirely new approach with no current treatments able to change scar in this way,” says Associate Professor James Chong who led the research. “By improving cardiac function and scar formation following heart attack, treatment with rhPDGF-AB led to an overall increase in survival rate in our study.”
“This is an entirely new approach with no current treatments able to change scar in this way,” says Associate Professor James Chong who led the research. “By improving cardiac function and scar formation following heart attack, treatment with rhPDGF-AB led to an overall increase in survival rate in our study.”

 …the researchers demonstrated that the biggest drop in cognitive ability occurs at the slightest level of hearing loss — a decline from zero to the “normal” level of 25 decibels, with smaller cognitive losses occurring when hearing deficits rise from 25 to 50 decibels.
…the researchers demonstrated that the biggest drop in cognitive ability occurs at the slightest level of hearing loss — a decline from zero to the “normal” level of 25 decibels, with smaller cognitive losses occurring when hearing deficits rise from 25 to 50 decibels.
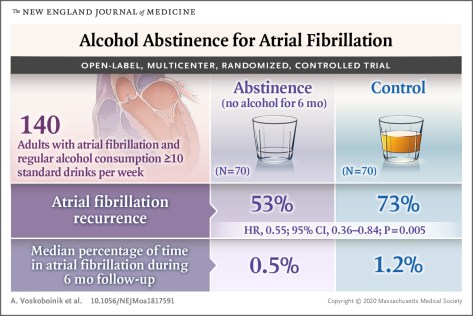
 When the five sleep factors were collapsed into binary categories of low risk vs. high risk (reference group), early chronotype, adequate sleep duration, free of insomnia, and no frequent daytime sleepiness were each independently associated with incident CVD, with a 7%, 12%, 8%, and 15% lower risk, respectively (Table
When the five sleep factors were collapsed into binary categories of low risk vs. high risk (reference group), early chronotype, adequate sleep duration, free of insomnia, and no frequent daytime sleepiness were each independently associated with incident CVD, with a 7%, 12%, 8%, and 15% lower risk, respectively (Table 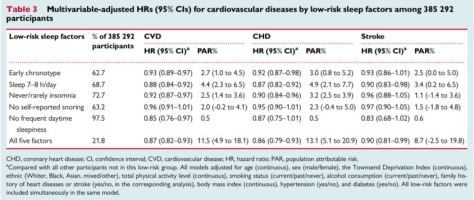 Cardiovascular disease (CVD), including coronary heart disease (CHD) and stroke, is among the leading causes of mortality globally.
Cardiovascular disease (CVD), including coronary heart disease (CHD) and stroke, is among the leading causes of mortality globally.