From U.S. News (July 7, 2020):
“Numerous studies have linked insufficient sleep with significant health consequences. Yet, many people ignore the signs of sleep problems or don’t allow enough time to get adequate sleep,” said lead researcher Eileen Leary. She is a senior manager of clinical research at Stanford University in Palo Alto, Calif.
“REM sleep appears to be a reliable predictor of mortality and may have other predictive health values,” Leary said. “Strategies to preserve REM may influence clinical therapies and reduce mortality risk, particularly for adults with less than 15% of REM sleep.”
REM (rapid eye movement) sleep is when dreams occur and the body repairs itself from the ravages of the day. For every 5% reduction in REM sleep, mortality rates increase 13% to 17% among older and middle-aged adults, researchers report.
For the study, Leary and her colleagues included more than 2,600 men, average age 76, who were followed for a median of 12 years. They also collected data on nearly 1,400 men and women, average age 52, who were part of another study and were followed for a median of 21 years.
Poor REM sleep was tied to early death from any cause as well as death from cardiovascular and other diseases, the researchers found.



 “We’ve discovered that fragmented sleep is associated with a unique pathway — chronic circulating inflammation throughout the blood stream — which, in turn, is linked to higher amounts of plaques in coronary arteries,” said study senior author Matthew Walker, a UC Berkeley professor of psychology and neuroscience.
“We’ve discovered that fragmented sleep is associated with a unique pathway — chronic circulating inflammation throughout the blood stream — which, in turn, is linked to higher amounts of plaques in coronary arteries,” said study senior author Matthew Walker, a UC Berkeley professor of psychology and neuroscience.
 The association between poor overall sleep quality and greater consumption of added sugars observed in the current study aligns with previous findings that intakes of confectionary and sugar‐sweetened beverages were higher in middle‐aged Japanese women reporting poor, compared with good, sleep quality.
The association between poor overall sleep quality and greater consumption of added sugars observed in the current study aligns with previous findings that intakes of confectionary and sugar‐sweetened beverages were higher in middle‐aged Japanese women reporting poor, compared with good, sleep quality.
 When the five sleep factors were collapsed into binary categories of low risk vs. high risk (reference group), early chronotype, adequate sleep duration, free of insomnia, and no frequent daytime sleepiness were each independently associated with incident CVD, with a 7%, 12%, 8%, and 15% lower risk, respectively (Table
When the five sleep factors were collapsed into binary categories of low risk vs. high risk (reference group), early chronotype, adequate sleep duration, free of insomnia, and no frequent daytime sleepiness were each independently associated with incident CVD, with a 7%, 12%, 8%, and 15% lower risk, respectively (Table 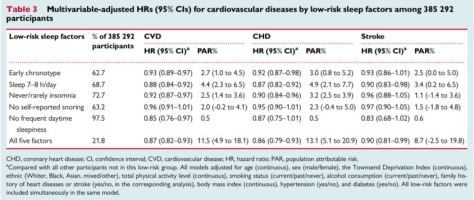 Cardiovascular disease (CVD), including coronary heart disease (CHD) and stroke, is among the leading causes of mortality globally.
Cardiovascular disease (CVD), including coronary heart disease (CHD) and stroke, is among the leading causes of mortality globally.

 “There are two important takeaways from this paper. One is that poor sleep is associated with brain immune dysregulation or dysfunction,” says Lim, the corresponding author for the paper.
“There are two important takeaways from this paper. One is that poor sleep is associated with brain immune dysregulation or dysfunction,” says Lim, the corresponding author for the paper.
 Sleep problems may decrease the likelihood of recovery from chronic low
Sleep problems may decrease the likelihood of recovery from chronic low  The current study points to the role of norepinephrine, a neurotransmitter that signals arousal and stress in the central nervous system. This chemical is present in low levels in the brain while we sleep, but when production ramps up it arouses our nerve cells, causing us to wake up and become alert. The study showed that norepinephrine also acts on a specific receptor, the beta2 adrenergic receptor, which is expressed at high levels in microglia. When this chemical is present in the brain, the microglia slip into a sort of hibernation.
The current study points to the role of norepinephrine, a neurotransmitter that signals arousal and stress in the central nervous system. This chemical is present in low levels in the brain while we sleep, but when production ramps up it arouses our nerve cells, causing us to wake up and become alert. The study showed that norepinephrine also acts on a specific receptor, the beta2 adrenergic receptor, which is expressed at high levels in microglia. When this chemical is present in the brain, the microglia slip into a sort of hibernation. …these results indicate that sleep may play an important role in health disparities and may represent a modifiable risk factor (along with diet and physical activity) for cardiometabolic risk in general and cardiometabolic health disparities specifically.
…these results indicate that sleep may play an important role in health disparities and may represent a modifiable risk factor (along with diet and physical activity) for cardiometabolic risk in general and cardiometabolic health disparities specifically. PBHWB of 40–42.5 °C was associated with both improved self-rated sleep quality and SE, and when scheduled 1–2 h before bedtime for little as 10 min significant shortening of SOL. These findings are consistent with the mechanism of PBHWB effects being the extent of core body temperature decline achieved by increased blood perfusion to the palms and soles that augments the distal-to-proximal skin temperature gradient to enhance body heat
PBHWB of 40–42.5 °C was associated with both improved self-rated sleep quality and SE, and when scheduled 1–2 h before bedtime for little as 10 min significant shortening of SOL. These findings are consistent with the mechanism of PBHWB effects being the extent of core body temperature decline achieved by increased blood perfusion to the palms and soles that augments the distal-to-proximal skin temperature gradient to enhance body heat 
