Taking a statin helps keep your cholesterol levels in check. How can that be?
 Dr. Stephen Kopecky explains that some people ask to be put on a statin. That’s because statins, while important and effective, are just one part of the whole heart-healthy picture. When you combine a statin with regular exercise, maintaining a healthy weight, controlling stress, not smoking and eating foods based on the Mediterranean diet, you can improve your heart health.
Dr. Stephen Kopecky explains that some people ask to be put on a statin. That’s because statins, while important and effective, are just one part of the whole heart-healthy picture. When you combine a statin with regular exercise, maintaining a healthy weight, controlling stress, not smoking and eating foods based on the Mediterranean diet, you can improve your heart health.
Dr. Kopecky says if you work in lifestyle changes slowly over time, you’ll be on your way to better heart health.
Statins are drugs that can lower your cholesterol. They work by blocking a substance your body needs to make cholesterol. Statins may also help your body reabsorb cholesterol that has built up in plaques on your artery walls, preventing further blockage in your blood vessels and heart attacks.
Several statins are available for use in the United States. They include:
- atorvastatin (Lipitor)
- lovastatin (Altoprev)
- pitavastatin (Livalo)
- pravastatin (Pravachol)
- rosuvastatin (Crestor)
- simvastatin (Zocor)
Sometimes, a statin is combined with another heart health medication. Examples are atorvastatin/amlodipine (Caduet) and simvastatin/ezetimibe (Vytorin).
Increasing evidence suggests that statins do more than just lower bad cholesterol. Research has found that the medicines can safely prevent heart disease in certain adults ages 40 to 75. But the benefits aren’t entirely clear for the elderly. And doctors still want to know more about the side effects of statins.






 The intake of marine omega-3s has consistently been found to have antiarrhythmic effects. When marine omega-3s are consumed, there is an increase in cellular membrane fluidity, inhibition of L-type calcium channels and a reduction in the chance of arrhythmic events during susceptible times. Prospective data suggest that maintaining an omega-3 index of about 8%, which requires consuming seafood rich in omega-3 up to five times per week or consuming over 3 g of EPA and DHA per day, may provide the greatest protection against arrhythmic events.
The intake of marine omega-3s has consistently been found to have antiarrhythmic effects. When marine omega-3s are consumed, there is an increase in cellular membrane fluidity, inhibition of L-type calcium channels and a reduction in the chance of arrhythmic events during susceptible times. Prospective data suggest that maintaining an omega-3 index of about 8%, which requires consuming seafood rich in omega-3 up to five times per week or consuming over 3 g of EPA and DHA per day, may provide the greatest protection against arrhythmic events.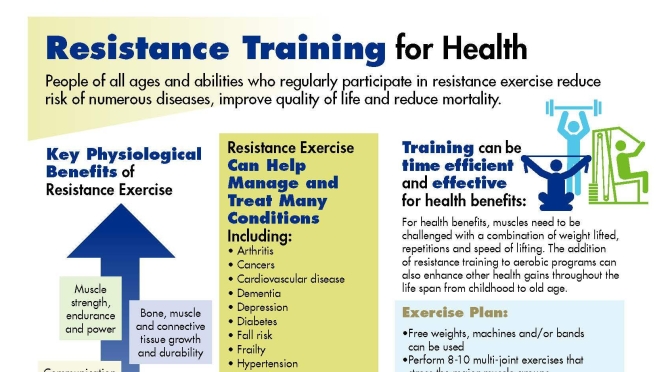
 The 10 year CVD (cardiovascular disease) incidence increased significantly across the baseline SMI (skeletal muscle mass index) tertiles (p<0.001). Baseline SMM (Skeletal muscle mass) showed a significant inverse association with the 10 year CVD incidence (HR 0.06, 95% CI 0.005 to 0.78), even after adjusting for various confounders. Additionally, participants in the highest SMM tertile had 81% (95% CI 0.04 to 0.85) lower risk for a CVD event as compared with those in the lowest SMM tertile.
The 10 year CVD (cardiovascular disease) incidence increased significantly across the baseline SMI (skeletal muscle mass index) tertiles (p<0.001). Baseline SMM (Skeletal muscle mass) showed a significant inverse association with the 10 year CVD incidence (HR 0.06, 95% CI 0.005 to 0.78), even after adjusting for various confounders. Additionally, participants in the highest SMM tertile had 81% (95% CI 0.04 to 0.85) lower risk for a CVD event as compared with those in the lowest SMM tertile.


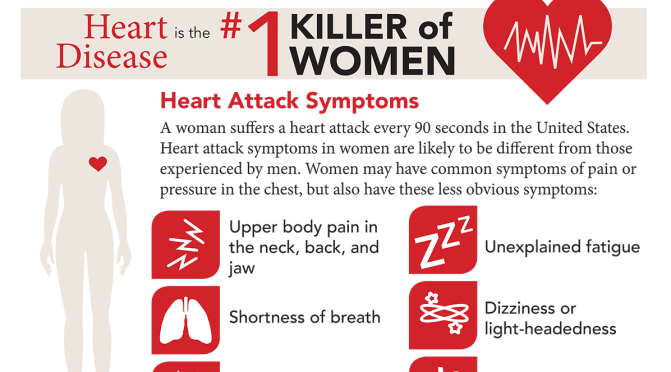
 “Our data showed that rates of accelerating blood pressure elevation were significantly higher in women than men, starting earlier in life,” said Cheng, the Erika J. Glazer Chair in Women’s Cardiovascular Health, who also serves as director of Cardiovascular Population Sciences at the Barbra Streisand Women’s Heart Center. “This means that if we define the hypertension threshold the exact same way, a 30-year old woman with high blood pressure is probably at higher risk for cardiovascular disease than a man with high blood pressure at the same age.”
“Our data showed that rates of accelerating blood pressure elevation were significantly higher in women than men, starting earlier in life,” said Cheng, the Erika J. Glazer Chair in Women’s Cardiovascular Health, who also serves as director of Cardiovascular Population Sciences at the Barbra Streisand Women’s Heart Center. “This means that if we define the hypertension threshold the exact same way, a 30-year old woman with high blood pressure is probably at higher risk for cardiovascular disease than a man with high blood pressure at the same age.”

 Death rates from cardiovascular disease among people between the ages of 45 and 64 are rising in cities all across the country, including in some of the most unlikely places.
Death rates from cardiovascular disease among people between the ages of 45 and 64 are rising in cities all across the country, including in some of the most unlikely places.