
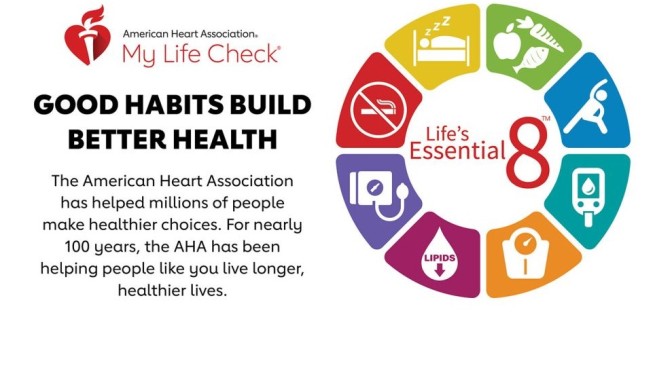
October 2022 – The American Heart Association (AHA) recently revised its checklist for achieving optimal heart health, introducing its new Life’s Essential 8. The list replaces the AHA’s decade-old Life’s Simple 7.
Sleep health is the new addition to the cardiovascular health scoring tool, which now advises that adults get seven to nine hours per night. The organization updated four of the categories:
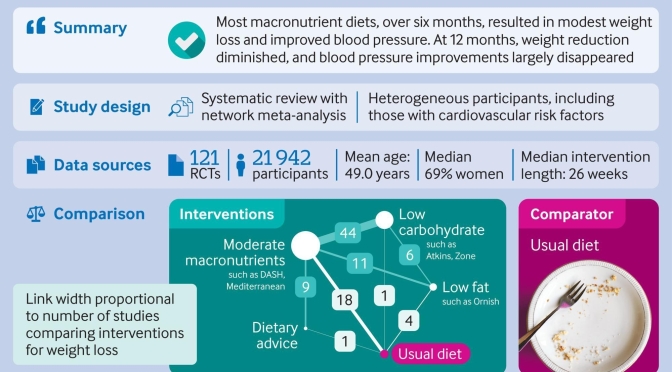
- Diet: More emphasis was given to following heart-healthy diets like the DASH and Mediterranean.
- Nicotine exposure: Secondhand smoke and vaping were added as risk factors.
- Blood lipids: People now can get a non-fasting blood sample that measures total, HDL, and non-HDL cholesterol. Non-HDL cholesterol can provide similar risk information as LDL cholesterol.
- Blood sugar: Measurements now include hemoglobin A1c, a key component to assessing type 2 diabetes risk.
- Three categories were unchanged:
- Physical activity: The optimal weekly level is at least 150 minutes of moderate activity or 75 minutes of vigorous activity.
- Body mass index (BMI): A BMI of 18.5 to 24.9 is ideal for heart health.
- Blood pressure: Levels less than 120/80 millimeters of mercury (mm Hg) remain optimal. Stage 1 hypertension is 130 to 139 mm Hg for systolic pressure (the first number) or 80 to 89 mm Hg for diastolic pressure (the second number).
- You can calculate your heart health score at mlc.heart.org. The guidelines were published online June 29, 2022, by Circulation.








 patrolling neighborhoods, or military soldiers during field-exercises. Thus, time-restricted eating removes the added stress of what to eat, and serves as a practical intervention conducive to the schedules of many people.
patrolling neighborhoods, or military soldiers during field-exercises. Thus, time-restricted eating removes the added stress of what to eat, and serves as a practical intervention conducive to the schedules of many people.

 Seasonal variation in blood pressure has been known for 40 years, but, to our knowledge, for the first time we show here that this occurs independently of temperature. The reduction in blood pressure is more marked with a rise in UVB than UVA, and in whites than black people. Dermatological concerns about the skin cancer inducing effects of UV radiation need to be balanced against the observed blood pressure lowering effects of sunlight, particularly given the greatly higher burden of disease caused by hypertension.
Seasonal variation in blood pressure has been known for 40 years, but, to our knowledge, for the first time we show here that this occurs independently of temperature. The reduction in blood pressure is more marked with a rise in UVB than UVA, and in whites than black people. Dermatological concerns about the skin cancer inducing effects of UV radiation need to be balanced against the observed blood pressure lowering effects of sunlight, particularly given the greatly higher burden of disease caused by hypertension. Sunlight exposure appears to lower blood pressure; insufficient exposure to natural ultraviolet radiation and/or active avoidance of sunlight may be new risk factors for hypertension.
Sunlight exposure appears to lower blood pressure; insufficient exposure to natural ultraviolet radiation and/or active avoidance of sunlight may be new risk factors for hypertension.