



The US Surgeon General’s office has released a report emphasizing the importance of making hypertension control a national public health priority. Vice Admiral Jerome Adams, MD, MPH, the 20th US Surgeon General, discusses the report’s background and recommendations.
Recorded October 7, 2020.


 Chest pain is a common chief complaint. It may be caused by either benign or life-threatening aetiologies and is usually divided into cardiac and non-cardiac causes. James E. Brown, Professor and Chair, Wright State University Boonshoft School of Medicine, Kettering, Ohio, gives us an overview of assessing chest pain in the emergency setting.
Chest pain is a common chief complaint. It may be caused by either benign or life-threatening aetiologies and is usually divided into cardiac and non-cardiac causes. James E. Brown, Professor and Chair, Wright State University Boonshoft School of Medicine, Kettering, Ohio, gives us an overview of assessing chest pain in the emergency setting.
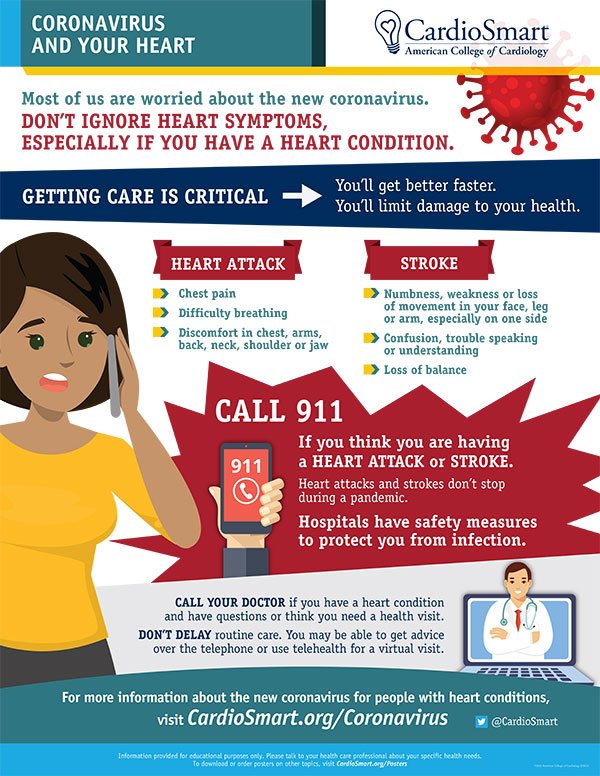
Hospitals across the U.S. are experiencing an influx of COVID-19 patients, but clinicians are reportedly seeing fewer patients going to the emergency room for heart attack or stroke.
Experts worry that patients who need critical care are delaying their treatment over COVID-19 concerns.
To encourage patients to pay close attention to their symptoms and call 9-1-1 immediately if they believe they are having a heart attack or stroke, ACC’s CardioSmart team developed the Coronavirus and Your Heart Infographic.
The infographic urges patients not to ignore symptoms, especially if they have a heart condition, and reassures them that hospitals have safety measures to protect patients from infection with the novel coronavirus.
From a BMJ Research study (March 4, 2020):
 Habitual fish oil supplementation is associated with a 13% lower risk of all cause mortality, a 16% lower risk of CVD mortality, and a 7% lower risk of CVD events among the general population
Habitual fish oil supplementation is associated with a 13% lower risk of all cause mortality, a 16% lower risk of CVD mortality, and a 7% lower risk of CVD events among the general population
Fish oil is a rich source of long chain omega 3 fatty acids, a group of polyunsaturated fats that primarily include eicosapentaenoic acid and docosahexaenoic acid. Initially, these compounds were recommended for daily omega 3 fatty acid supplementation for the prevention of cardiovascular disease (CVD). Consequently, the use of fish oil supplements is widespread in the United Kingdom and other developed countries.

Several mechanisms could explain the benefits for clinical outcome derived from fish oil supplementation. Firstly, the results of several studies have indicated that supplementation with omega 3 fatty acids has beneficial effects on blood pressure, plasma triglycerides, and heart rate, all of which would exert a protective effect against the development of CVD. Secondly, several trials have shown that omega 3 fatty acids can improve flow mediated arterial dilatation, which is a measure of endothelial function and health. Thirdly, omega 3 fatty acids have been shown to possess antiarrhythmic properties that could be clinically beneficial. Finally, studies have reported that fish oil can reduce thrombosis. Additionally, studies have reported that the anti-inflammatory properties of fish oil could have a preventive role in the pathophysiology of CVD outcomes. Other mechanisms could also be involved to explain the effect of fish oil on CVD outcomes.
Hazen and colleagues find that gut bacteria play a central role in the conversion of dietary proteins into a compound, phenylacetylglutamine ( PAGln), which not only is associated with future cardiovascular disease risk in humans but also promotes platelet responsiveness and blood clotting potentially via adrenergic receptors, according to mouse models.
From an American Heart Assoc. Journal study (Feb 28, 2020):
 Seasonal variation in blood pressure has been known for 40 years, but, to our knowledge, for the first time we show here that this occurs independently of temperature. The reduction in blood pressure is more marked with a rise in UVB than UVA, and in whites than black people. Dermatological concerns about the skin cancer inducing effects of UV radiation need to be balanced against the observed blood pressure lowering effects of sunlight, particularly given the greatly higher burden of disease caused by hypertension.
Seasonal variation in blood pressure has been known for 40 years, but, to our knowledge, for the first time we show here that this occurs independently of temperature. The reduction in blood pressure is more marked with a rise in UVB than UVA, and in whites than black people. Dermatological concerns about the skin cancer inducing effects of UV radiation need to be balanced against the observed blood pressure lowering effects of sunlight, particularly given the greatly higher burden of disease caused by hypertension.
 Sunlight exposure appears to lower blood pressure; insufficient exposure to natural ultraviolet radiation and/or active avoidance of sunlight may be new risk factors for hypertension.
Sunlight exposure appears to lower blood pressure; insufficient exposure to natural ultraviolet radiation and/or active avoidance of sunlight may be new risk factors for hypertension.
Hypertension remains a leading global cause for premature death and disease. Most treatment guidelines emphasize the importance of risk factors, but not all are known, modifiable, or easily avoided. Population blood pressure correlates with latitude and is lower in summer than winter. Seasonal variations in sunlight exposure account for these differences, with temperature believed to be the main contributor. Recent research indicates that UV light enhances nitric oxide availability by mobilizing storage forms in the skin, suggesting incident solar UV radiation may lower blood pressure. We tested this hypothesis by exploring the association between environmental UV exposure and systolic blood pressure (SBP) in a large cohort of chronic hemodialysis patients in whom SBP is determined regularly.
From a “Circulation: Heart Failure” Journal study (Feb 25, 2020):
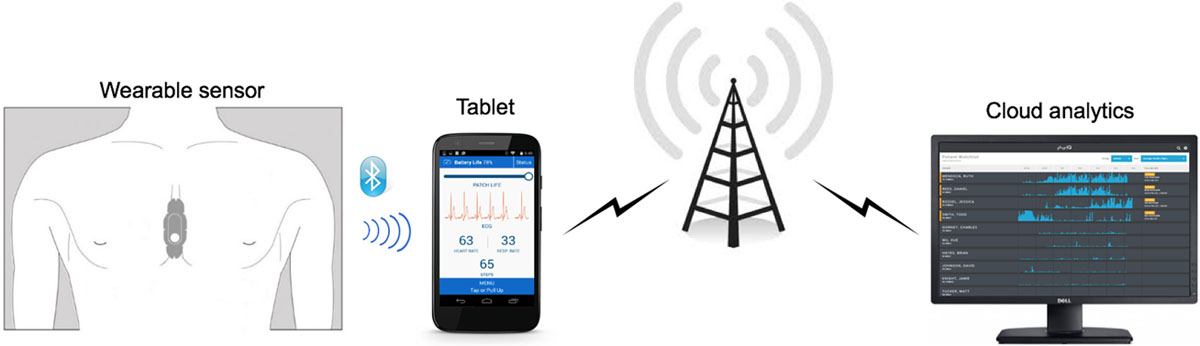
 The study shows that wearable sensors coupled with machine learning analytics have predictive accuracy comparable to implanted devices.
The study shows that wearable sensors coupled with machine learning analytics have predictive accuracy comparable to implanted devices.
We demonstrate that machine learning analytics using data from a wearable sensor can accurately predict hospitalization for heart failure exacerbation…at a median time of 6.5 days before the admission.
Heart failure (HF) is a major public health problem affecting >23 million patients worldwide. Hospitalization costs for HF represent 80% of costs attributed to HF care. Thus, accurate and timely detection of worsening HF could allow for interventions aimed at reducing the risk of HF admission.
Several such approaches have been tested. Tracking of daily weight, as recommended by current HF guidelines, did not lead to reduction of the risk of HF hospitalization, most likely because the weight gain is a contemporaneous or lagging indicator rather than a leading event. Interventions based on intrathoracic impedance monitoring also did not result in reduction of readmission risk. The results suggest that physiological parameters other than weight or intrathoracic impedance in isolation may be needed to detect HF decompensation in a timely manner. In fact, 28% reduction of rehospitalization rates has been shown with interventions based on pulmonary artery hemodynamic monitoring. More recently, in the MultiSENSE study (Multisensor Chronic Evaluation in Ambulatory HF Patients), an algorithm based on physiological data from sensors in the implantable cardiac resynchronization therapy defibrillators, was shown to have 70% sensitivity in predicting the risk of HF hospitalization or outpatient visit with intravenous therapies for worsening of HF.