Medical wearables are quickly becoming a potential solution in a world where tele-health is gaining ground. Here are three examples of challenges in designing medical wearables, and how to overcome them.
Tag Archives: Wearable Sensors
Digital Health: The Future Of Wearable Devices


Currently, smartwatches provide information such as heart rate, sleep time and activity patterns. In the future, this could be augmented with new classes of wearable devices that monitor, for example, concentrations of cortisol for tracking stress (using electronic epidermal tattoos), biomarkers of inflammation and levels of blood O2 (microneedle patches), skin temperature (electronic textiles), blood pressure (smart rings), concentration of ions (wristbands), intraocular pressure (smart contact lenses), the presence of airborne pathogens and breathing anomalies (face masks), and the concentration of therapeutic drugs (on-teeth sensors)2,10,12,13,14,15,16. Such emerging low-cost wearable sensing technologies, monitoring both physical parameters and biochemical markers, could be used to identify symptomatic and pre-symptomatic cases in future pandemics. The devices could also be used to remotely monitor the recovery of individuals undergoing treatment or self-isolating at home.
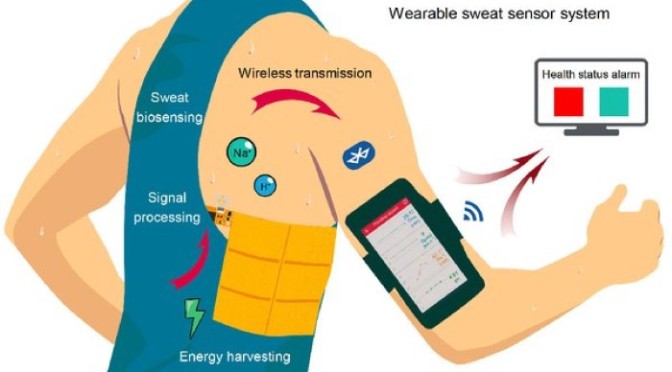
Innovations: ‘Wireless Wearable Health Sensor’ Is Human Motion Powered
Gao has developed a new way to power wireless wearable sensors: He harvests kinetic energy that is produced by a person as they move around.

“Our triboelectric generator, also called a nanogenerator, has a stator, which is fixed to the torso, and a slider, which is attached to the inside of the arm. The slider slides against the stator during human motion, and, an electrical current is generated at the same time,” Gao says. “The mechanism is quite simple. Friction results in electrical generation. This is not something new, concept-wise.”

This energy harvesting is done with a thin sandwich of materials (Teflon, copper, and polyimide) that are attached to the person’s skin. As the person moves, these sheets of material rub against a sliding layer made of copper and polyimide, and generate small amounts of electricity. The effect, known as triboelectricity, is perhaps best illustrated by the static electric shock a person might receive after walking across a carpeted floor and then touching a metal doorknob.
Digital Health: Wearable Sensor Data Can Predict Heart Failure 6 Days Before Hospitalization
From a “Circulation: Heart Failure” Journal study (Feb 25, 2020):
 The study shows that wearable sensors coupled with machine learning analytics have predictive accuracy comparable to implanted devices.
The study shows that wearable sensors coupled with machine learning analytics have predictive accuracy comparable to implanted devices.
We demonstrate that machine learning analytics using data from a wearable sensor can accurately predict hospitalization for heart failure exacerbation…at a median time of 6.5 days before the admission.
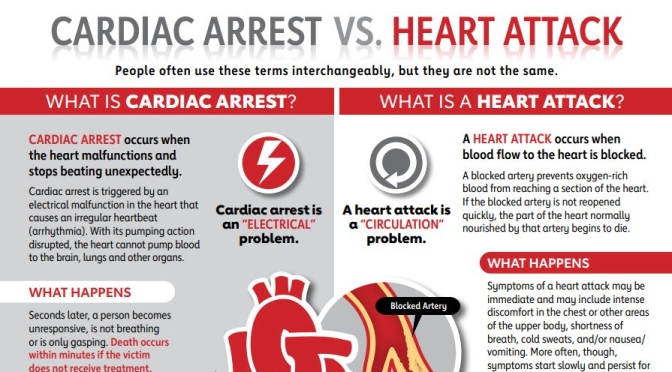
Heart failure (HF) is a major public health problem affecting >23 million patients worldwide. Hospitalization costs for HF represent 80% of costs attributed to HF care. Thus, accurate and timely detection of worsening HF could allow for interventions aimed at reducing the risk of HF admission.

Several such approaches have been tested. Tracking of daily weight, as recommended by current HF guidelines, did not lead to reduction of the risk of HF hospitalization, most likely because the weight gain is a contemporaneous or lagging indicator rather than a leading event. Interventions based on intrathoracic impedance monitoring also did not result in reduction of readmission risk. The results suggest that physiological parameters other than weight or intrathoracic impedance in isolation may be needed to detect HF decompensation in a timely manner. In fact, 28% reduction of rehospitalization rates has been shown with interventions based on pulmonary artery hemodynamic monitoring. More recently, in the MultiSENSE study (Multisensor Chronic Evaluation in Ambulatory HF Patients), an algorithm based on physiological data from sensors in the implantable cardiac resynchronization therapy defibrillators, was shown to have 70% sensitivity in predicting the risk of HF hospitalization or outpatient visit with intravenous therapies for worsening of HF.