
Opportunities for enhancing brain health across the lifespan
Published online by Cambridge University Press: 22 March 2021
Summary
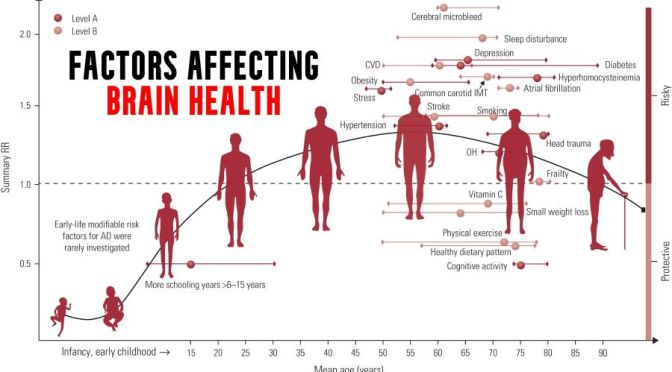
As we age, there are characteristic changes in our thinking, reasoning and memory skills (referred to as cognitive ageing). However, variation between people in the timing and degree of change experienced suggests that a range of factors determine individual cognitive ageing trajectories. This narrative review considers some of the lifestyle factors that might promote (or harm) cognitive health. The focus on lifestyle factors is because these are potentially modifiable by individuals or may be the targets of behavioural or societal interventions. To support that, the review briefly considers people’s beliefs and attitudes about cognitive ageing; the nature and timing of cognitive changes across the lifespan; and the genetic contributions to cognitive ability level and change. In introducing potentially modifiable determinants, a framing that draws evidence derived from epidemiological studies of dementia is provided, before an overview of lifestyle and behavioural predictors of cognitive health, including education and occupation, diet and activity.




 Even limited hearing loss might be associated with cognitive decline. If true, early intervention with hearing aids might help people have better cognitive performance.
Even limited hearing loss might be associated with cognitive decline. If true, early intervention with hearing aids might help people have better cognitive performance. 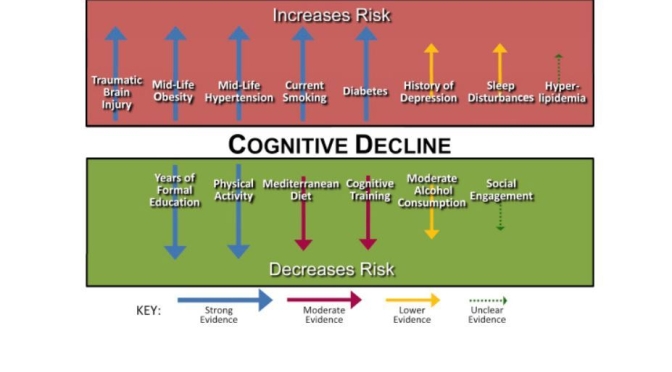
 This relationship between higher glucose levels and poorer cognitive functioning extended beyond just CASI z-score, as well, Cukierman-Yaffe noted. Higher HbA1c levels were also tied to significantly poorer performance in other psychological tests, including the clock making test of executive functioning, test of discriminative ability, and for the test of verbal fluency.
This relationship between higher glucose levels and poorer cognitive functioning extended beyond just CASI z-score, as well, Cukierman-Yaffe noted. Higher HbA1c levels were also tied to significantly poorer performance in other psychological tests, including the clock making test of executive functioning, test of discriminative ability, and for the test of verbal fluency.

 First place prize awarded to MapHabit: This mobile software provides behavior prompts with customizable picture and keyword visual maps to assist memory-impaired people with accomplishing activities of daily living. The care management platform employs different interfaces depending on whether the user is a person with impaired memory, caregiver or long-term care community manager. Caregivers can monitor adherence to medication schedules or track other activities.
First place prize awarded to MapHabit: This mobile software provides behavior prompts with customizable picture and keyword visual maps to assist memory-impaired people with accomplishing activities of daily living. The care management platform employs different interfaces depending on whether the user is a person with impaired memory, caregiver or long-term care community manager. Caregivers can monitor adherence to medication schedules or track other activities.
 The team found 85% of people first diagnosed with dementia were diagnosed by a non-dementia specialist physician, usually a primary care doctor, and an “unspecified dementia” diagnosis was common.
The team found 85% of people first diagnosed with dementia were diagnosed by a non-dementia specialist physician, usually a primary care doctor, and an “unspecified dementia” diagnosis was common.
 In our study, we found significant associations between baseline teeth symptoms and change in episodic memory. Deficits in episodic memory (ie, ability to retain new information) are most common in older adults with mild cognitive impairment making them more likely to progress to Alzheimer’s disease dementia.
In our study, we found significant associations between baseline teeth symptoms and change in episodic memory. Deficits in episodic memory (ie, ability to retain new information) are most common in older adults with mild cognitive impairment making them more likely to progress to Alzheimer’s disease dementia.