From a MedPage Today online article (April 2, 2020):
 This relationship between higher glucose levels and poorer cognitive functioning extended beyond just CASI z-score, as well, Cukierman-Yaffe noted. Higher HbA1c levels were also tied to significantly poorer performance in other psychological tests, including the clock making test of executive functioning, test of discriminative ability, and for the test of verbal fluency.
This relationship between higher glucose levels and poorer cognitive functioning extended beyond just CASI z-score, as well, Cukierman-Yaffe noted. Higher HbA1c levels were also tied to significantly poorer performance in other psychological tests, including the clock making test of executive functioning, test of discriminative ability, and for the test of verbal fluency.
Poorer glycemic control was tied to cognitive decline following a lacunar stroke in a prospective cohort study.
Among 942 individuals with type 2 diabetes who had a lacunar stroke, every 1% higher HbA1c was tied to a 0.06 drop in cognitive function at baseline measured by Cognitive Assessment Screening Instrument (CASI) z-score (95% CI -0.101 to -0.018), reported Tali Cukierman-Yaffe, MD, MSc, of Sheba Medical Center and the Sackler School of Medicine of Tel Aviv University in Israel.
Read more
 Even limited hearing loss might be associated with cognitive decline. If true, early intervention with hearing aids might help people have better cognitive performance.
Even limited hearing loss might be associated with cognitive decline. If true, early intervention with hearing aids might help people have better cognitive performance. 



 This relationship between higher glucose levels and poorer cognitive functioning extended beyond just CASI z-score, as well, Cukierman-Yaffe noted. Higher HbA1c levels were also tied to significantly poorer performance in other psychological tests, including the clock making test of executive functioning, test of discriminative ability, and for the test of verbal fluency.
This relationship between higher glucose levels and poorer cognitive functioning extended beyond just CASI z-score, as well, Cukierman-Yaffe noted. Higher HbA1c levels were also tied to significantly poorer performance in other psychological tests, including the clock making test of executive functioning, test of discriminative ability, and for the test of verbal fluency.
 Across the 6 studies of 8699 participants, mean age ranged between 70 and 74 years and mean gait speed ranged between 1.05 and 1.26 m/s. Incident dementia ranged from 5 to 21 per 1000 person-years. Compared with usual agers, participants with only memory decline had 2.2 to 4.6 times higher risk for developing dementia…
Across the 6 studies of 8699 participants, mean age ranged between 70 and 74 years and mean gait speed ranged between 1.05 and 1.26 m/s. Incident dementia ranged from 5 to 21 per 1000 person-years. Compared with usual agers, participants with only memory decline had 2.2 to 4.6 times higher risk for developing dementia… 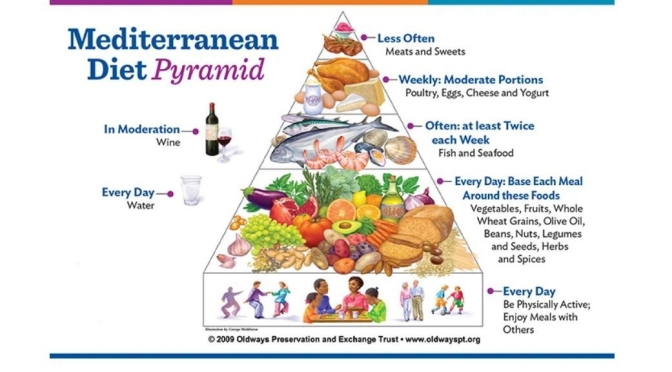
 We observed that increased adherence to the MedDiet modulates specific components of the gut microbiota that were associated with a reduction in risk of frailty, improved cognitive function and reduced inflammatory status.
We observed that increased adherence to the MedDiet modulates specific components of the gut microbiota that were associated with a reduction in risk of frailty, improved cognitive function and reduced inflammatory status.

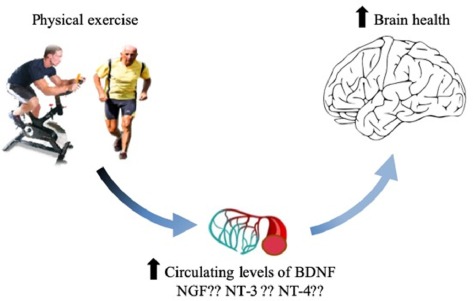
 In conclusion, increased CRF (cardiorespiratory fitness) following this six-month intervention was associated with enhanced brain glucose metabolism in the PCC (posterior cingulate cortex), a region linked to AD, and cognition among late-middle-aged individuals at risk for AD. If these findings are supported by a larger-scale study, this would provide strong evidence that adults at risk for AD may enhance brain function and cognition by engaging in aerobic exercise training.
In conclusion, increased CRF (cardiorespiratory fitness) following this six-month intervention was associated with enhanced brain glucose metabolism in the PCC (posterior cingulate cortex), a region linked to AD, and cognition among late-middle-aged individuals at risk for AD. If these findings are supported by a larger-scale study, this would provide strong evidence that adults at risk for AD may enhance brain function and cognition by engaging in aerobic exercise training.


 “There are two important takeaways from this paper. One is that poor sleep is associated with brain immune dysregulation or dysfunction,” says Lim, the corresponding author for the paper.
“There are two important takeaways from this paper. One is that poor sleep is associated with brain immune dysregulation or dysfunction,” says Lim, the corresponding author for the paper.