From the Wall Street Journal (June 8, 2020):
“We have to operate a hospital within a hospital, taking care of the needs for patients who have had strokes or a newborn delivery or need surgery while dealing with an otherwise healthy 35-year-old who picked up Covid-19 at a social event,” says James Linder, chief executive of Nebraska Medicine…
 For instance, more hospitals are remotely triaging and registering patients before they even arrive. Clinicians can consult with patients from their home via telemedicine to help determine how sick they are and if they need to come to the ER at all. From there, admissions are made with as little contact with staff or other patients as possible.
For instance, more hospitals are remotely triaging and registering patients before they even arrive. Clinicians can consult with patients from their home via telemedicine to help determine how sick they are and if they need to come to the ER at all. From there, admissions are made with as little contact with staff or other patients as possible.
Hospitals are rethinking how they operate in light of the Covid-19 pandemic—and preparing for a future where such crises may become a grim fact of life.
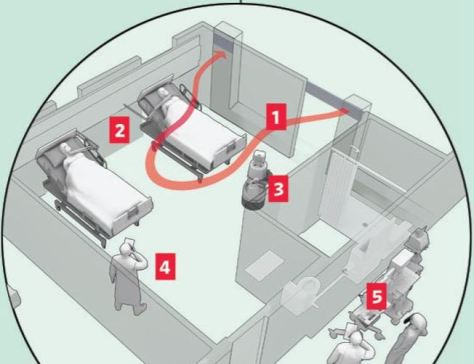
 With the potential for resurgences of the coronavirus, and some scientists warning about outbreaks of other infectious diseases, hospitals don’t want to be caught flat-footed again. So, more of them are turning to new protocols and new technology to overhaul standard operating procedure, from the time patients show up at an emergency room through admission, treatment and discharge.
With the potential for resurgences of the coronavirus, and some scientists warning about outbreaks of other infectious diseases, hospitals don’t want to be caught flat-footed again. So, more of them are turning to new protocols and new technology to overhaul standard operating procedure, from the time patients show up at an emergency room through admission, treatment and discharge.



 Ventilators have become prized in hospitals across the U.S. and beyond because they are desperately needed to treat very ill Covid-19 patients. But they are also feared for the damage they can inflict, and for the slim odds of survival they offer.
Ventilators have become prized in hospitals across the U.S. and beyond because they are desperately needed to treat very ill Covid-19 patients. But they are also feared for the damage they can inflict, and for the slim odds of survival they offer. 
 Facing shortages of critical equipment, medical workers must make life-or-death decisions about who receives care. WSJ’s Joe Palazzolo reports from an emergency room that’s running short on ventilators, and Chris Weaver explains the plans hospitals are putting in place to decide who gets them.
Facing shortages of critical equipment, medical workers must make life-or-death decisions about who receives care. WSJ’s Joe Palazzolo reports from an emergency room that’s running short on ventilators, and Chris Weaver explains the plans hospitals are putting in place to decide who gets them. 
 When he was interviewed, the count of Covid-19 cases stood at 412, less than 12 hours later, the new number was 505. He’s expecting the wave to hit hard there. Broward is home to Fort Lauderdale (think spring break) and Pompano Beach (think aging retirees). Couple those demographics with a lack of easy testing for the virus, and you’ve got a worrisome situation.
When he was interviewed, the count of Covid-19 cases stood at 412, less than 12 hours later, the new number was 505. He’s expecting the wave to hit hard there. Broward is home to Fort Lauderdale (think spring break) and Pompano Beach (think aging retirees). Couple those demographics with a lack of easy testing for the virus, and you’ve got a worrisome situation.
 Last year the Lancet published a paper on the impact of wearing gowns, surveying 928 adult patients and carrying out structured interviews with 10 patients. Over half (58%) reported wearing the gown despite feeling uncertain that it was a medical necessity. Gown design was considered inadequate, with 61% reporting that they struggled to put it on or required assistance and 67% reporting that it didn’t fit. Most worryingly, 72% felt exposed, 60% felt self-conscious, and 57% felt uncomfortable wearing the gown.
Last year the Lancet published a paper on the impact of wearing gowns, surveying 928 adult patients and carrying out structured interviews with 10 patients. Over half (58%) reported wearing the gown despite feeling uncertain that it was a medical necessity. Gown design was considered inadequate, with 61% reporting that they struggled to put it on or required assistance and 67% reporting that it didn’t fit. Most worryingly, 72% felt exposed, 60% felt self-conscious, and 57% felt uncomfortable wearing the gown.

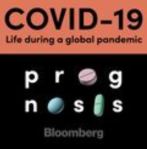
 High medical prices and billing practices may reduce public trust in the medical profession and can result in the avoidance of care. In a survey of 1000 patients, 64% reported that they delayed or neglected seeking medical care in the past year because of concern about high medical bills. The field of quality science in health care has developed measures of medical complications; however, there are no standardized metrics of billing quality.
High medical prices and billing practices may reduce public trust in the medical profession and can result in the avoidance of care. In a survey of 1000 patients, 64% reported that they delayed or neglected seeking medical care in the past year because of concern about high medical bills. The field of quality science in health care has developed measures of medical complications; however, there are no standardized metrics of billing quality. A recent study found that only 53 of 101 hospitals were able to provide a price for standard coronary artery bypass graft surgery. Notably, among the hospitals that provided a price, the price ranged from approximately $44 000 and $448 000 and was not associated with quality of care as measured by risk-adjusted outcomes and the Society of Thoracic Surgeons composite quality score.
A recent study found that only 53 of 101 hospitals were able to provide a price for standard coronary artery bypass graft surgery. Notably, among the hospitals that provided a price, the price ranged from approximately $44 000 and $448 000 and was not associated with quality of care as measured by risk-adjusted outcomes and the Society of Thoracic Surgeons composite quality score.

 This week on Prognosis, we look at one startup that’s trying to redesign care for some of the most vulnerable patients, taking into account the complex realities of their lives. The company is trying to improve care for people and communities the medical system often fails – and it believes that fixing those failures will not only make people healthier, it will also save money.
This week on Prognosis, we look at one startup that’s trying to redesign care for some of the most vulnerable patients, taking into account the complex realities of their lives. The company is trying to improve care for people and communities the medical system often fails – and it believes that fixing those failures will not only make people healthier, it will also save money.
