Executive summary
The number of older people, including those living with dementia, is rising, as younger age mortality declines. However, the age-specific incidence of dementia has fallen in many countries, probably because of improvements in education, nutrition, health care, and lifestyle changes.
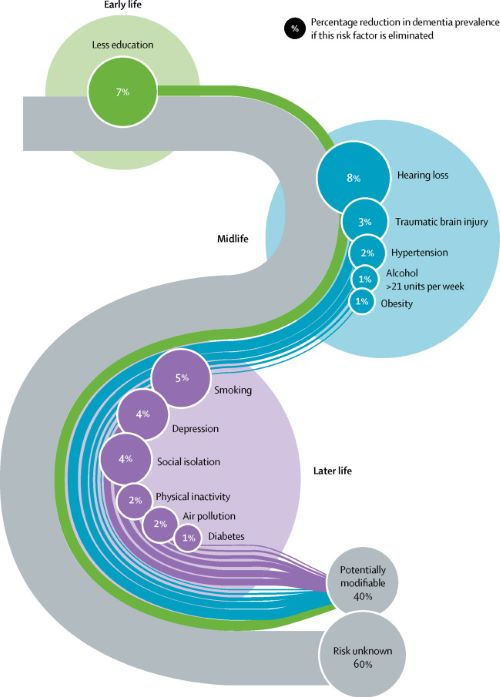
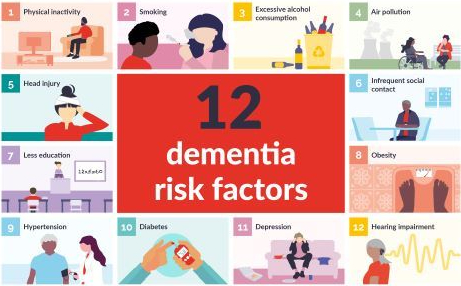
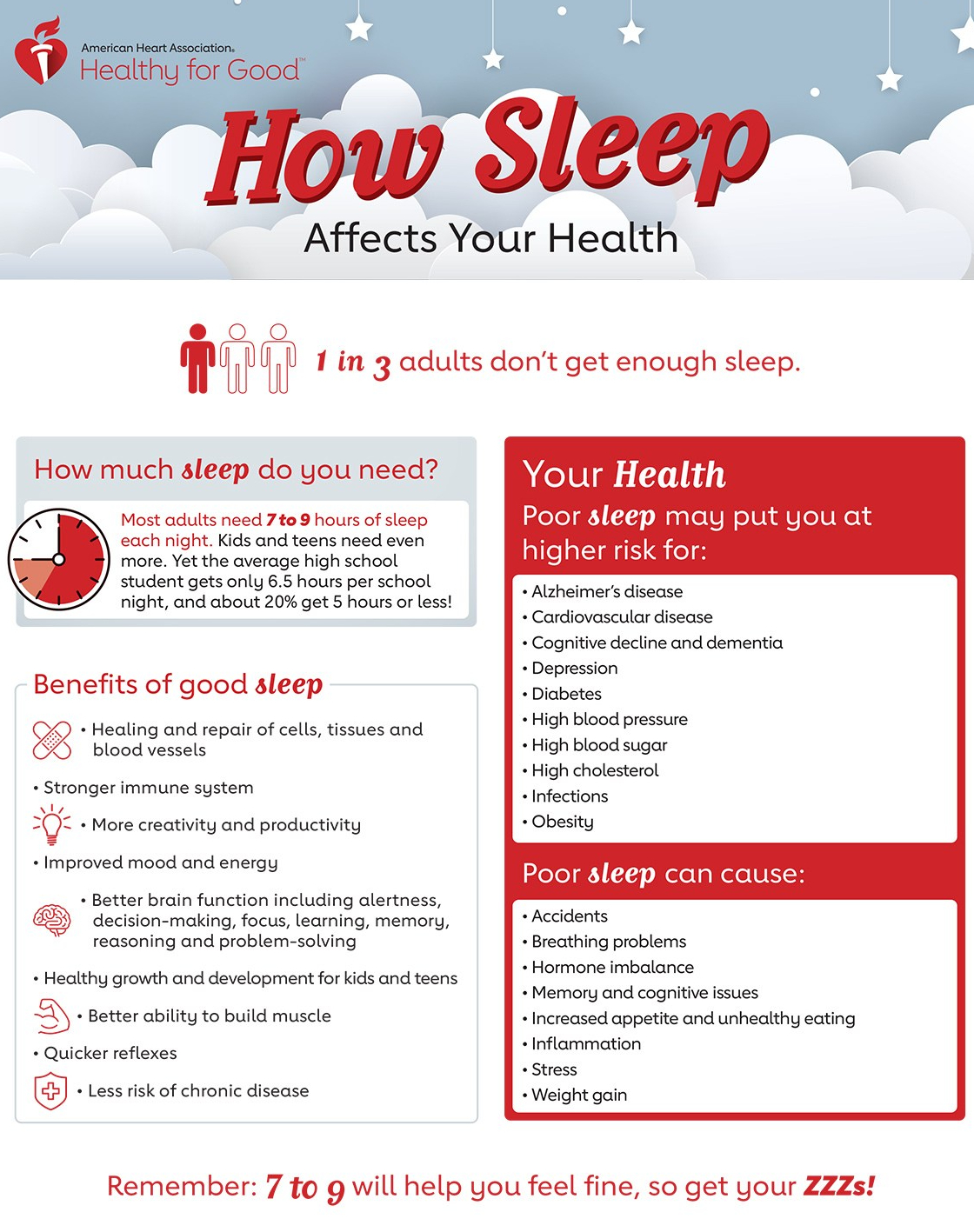
Overall, a growing body of evidence supports the nine potentially modifiable risk factors for dementia modelled by the 2017 Lancet Commission on dementia prevention, intervention, and care: less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, and low social contact.
We now add three more risk factors for dementia with newer, convincing evidence. These factors are excessive alcohol consumption, traumatic brain injury, and air pollution. We have completed new reviews and meta-analyses and incorporated these into an updated 12 risk factor life-course model of dementia prevention. Together the 12 modifiable risk factors account for around 40% of worldwide dementias, which consequently could theoretically be prevented or delayed.
The potential for prevention is high and might be higher in low-income and middle-income countries (LMIC) where more dementias occur. Our new life-course model and evidence synthesis has paramount worldwide policy implications. It is never too early and never too late in the life course for dementia prevention. Early-life (younger than 45 years) risks, such as less education, affect cognitive reserve; midlife (45–65 years), and later-life (older than 65 years) risk factors influence reserve and triggering of neuropathological developments.
Culture, poverty, and inequality are key drivers of the need for change. Individuals who are most deprived need these changes the most and will derive the highest benefit.




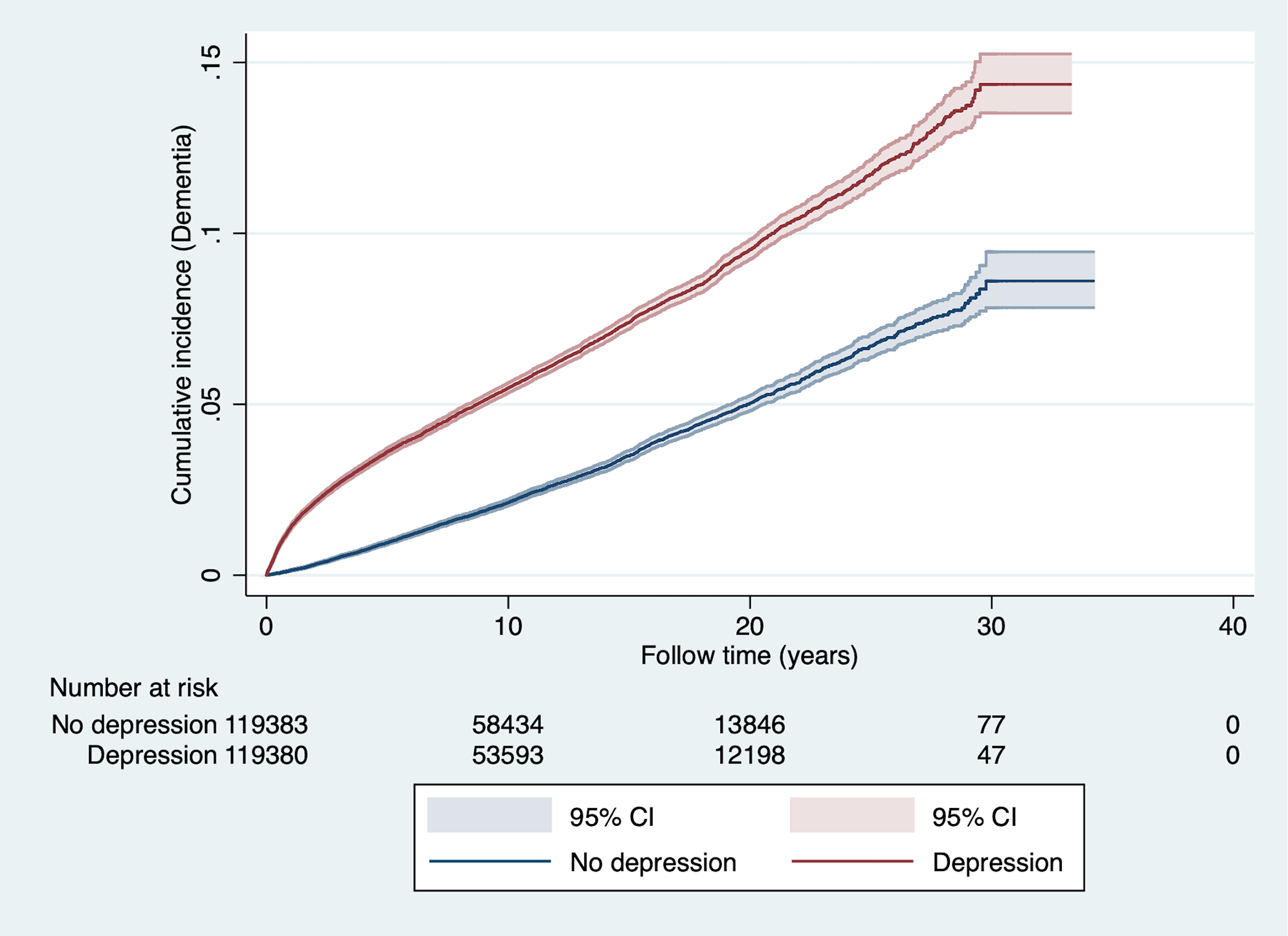
 We tested the hypothesis that apathy, but not depression, is associated with dementia in patients with SVD. We found that higher baseline apathy, as well as increasing apathy over time, were associated with an increased dementia risk. In contrast, neither baseline depression or change in depression was associated with dementia. The relationship between apathy and dementia remained after controlling for other well-established risk factors including age, education and cognition. Finally, adding apathy to models predicting dementia improved model fit. These results suggest that apathy may be a prodromal symptom of dementia in patients with SVD.
We tested the hypothesis that apathy, but not depression, is associated with dementia in patients with SVD. We found that higher baseline apathy, as well as increasing apathy over time, were associated with an increased dementia risk. In contrast, neither baseline depression or change in depression was associated with dementia. The relationship between apathy and dementia remained after controlling for other well-established risk factors including age, education and cognition. Finally, adding apathy to models predicting dementia improved model fit. These results suggest that apathy may be a prodromal symptom of dementia in patients with SVD.


 This systematic review and meta-analysis of 11 studies involving 21 517 physicians demonstrated an association between physician depressive symptoms and an increased risk for perceived medical errors (RR, 1.95; 95% CI, 1.63-2.33). We also found that the magnitude of the associations of physician depressive symptoms and perceived medical errors were relatively consistent across studies that assessed training and practicing physicians, providing additional evidence that physician depression has implications for the quality of care delivered by physicians at different career stages.
This systematic review and meta-analysis of 11 studies involving 21 517 physicians demonstrated an association between physician depressive symptoms and an increased risk for perceived medical errors (RR, 1.95; 95% CI, 1.63-2.33). We also found that the magnitude of the associations of physician depressive symptoms and perceived medical errors were relatively consistent across studies that assessed training and practicing physicians, providing additional evidence that physician depression has implications for the quality of care delivered by physicians at different career stages.
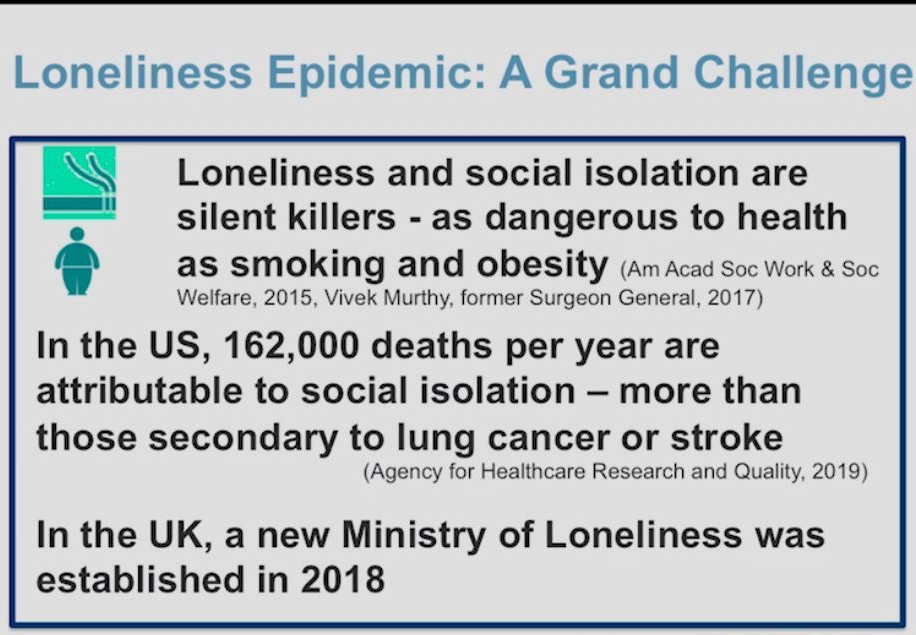 As societal stresses have increased, loneliness and social isolation have become silent killers. Dilip Jeste, MD, a geriatric neuropsychiatrist who specializes in successful aging, explains how loneliness has become an epidemic, the risk factors, helpful interventions, and how we can harness wisdom for compassion, self regulation, and more.
As societal stresses have increased, loneliness and social isolation have become silent killers. Dilip Jeste, MD, a geriatric neuropsychiatrist who specializes in successful aging, explains how loneliness has become an epidemic, the risk factors, helpful interventions, and how we can harness wisdom for compassion, self regulation, and more.
 The investigators discovered that patients with a higher genetic risk for depression were more likely to be diagnosed with depression over the next 2 years. However, more physically active patients at baseline were less likely to depression, even after they accounted for genetic risks.
The investigators discovered that patients with a higher genetic risk for depression were more likely to be diagnosed with depression over the next 2 years. However, more physically active patients at baseline were less likely to depression, even after they accounted for genetic risks.
 There may be no easy fix for the loneliness epidemic plaguing the nation, but helping people cope with hearing loss could be one key to tackling this complex problem. Hearing loss affects 1 of every 5 people and is strongly linked to loneliness: Every decibel drop in perception in people under 70 increases the odds of becoming severely lonely by 7%,
There may be no easy fix for the loneliness epidemic plaguing the nation, but helping people cope with hearing loss could be one key to tackling this complex problem. Hearing loss affects 1 of every 5 people and is strongly linked to loneliness: Every decibel drop in perception in people under 70 increases the odds of becoming severely lonely by 7%,