From the New England Journal of Medicine (February 13, 2020):
 In our opinion, the current recommendation to greatly increase consumption of dairy foods to 3 or more servings per day does not appear to be justified…When consumption of milk is low, the two nutrients of primary concern, calcium and vitamin D (which is of particular concern at higher latitudes), be obtained from other foods or supplements without the potential negative consequences of dairy foods.
In our opinion, the current recommendation to greatly increase consumption of dairy foods to 3 or more servings per day does not appear to be justified…When consumption of milk is low, the two nutrients of primary concern, calcium and vitamin D (which is of particular concern at higher latitudes), be obtained from other foods or supplements without the potential negative consequences of dairy foods.
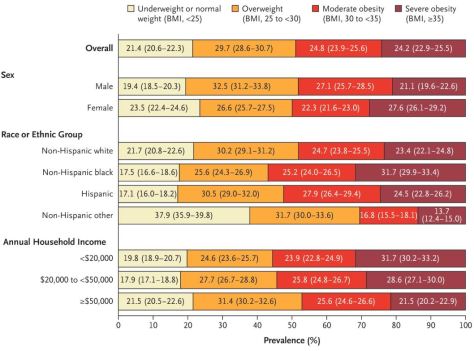
For calcium, alternative dietary sources include kale, broccoli, tofu, nuts, beans, and fortified orange juice for vitamin D, supplements can provide adequate intake at far lower cost than fortified milk. Pending additional research, guidelines for milk and equivalent dairy foods ideally should designate an acceptable intake (such as 0 to 2 servings per day for adults), deemphasize reduced-fat milk as preferable to whole milk, and discourage consumption of sugar-sweetened dairy foods in populations with high rates of overweight and obesity.
For adults, the overall evidence does not support high dairy consumption for reduction of fractures, which has been a primary justification for current U.S. recommendations. Moreover, total dairy consumption has not been clearly related to weight control or to risks of diabetes and cardiovascular disease. High consumption of dairy foods is likely to increase the risks of prostate cancer and possibly endometrial cancer but reduce the risk of colorectal cancer.


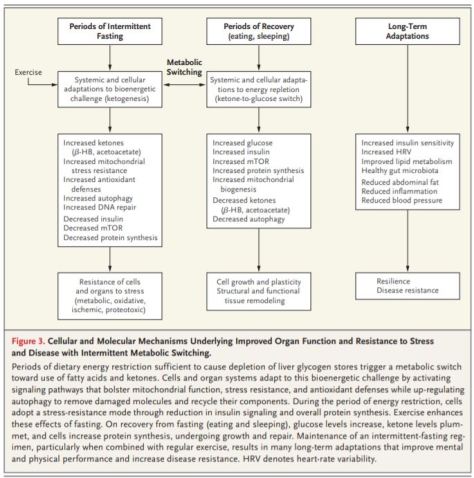
 Intermittent fasting has salutary effects. Listen how Dr. Mark P. Mattson, co-author of a recent NEJM review on the topic, assesses the practice — and how he’s managed to skip breakfast for the past 30 years or so.
Intermittent fasting has salutary effects. Listen how Dr. Mark P. Mattson, co-author of a recent NEJM review on the topic, assesses the practice — and how he’s managed to skip breakfast for the past 30 years or so.
 Featuring articles on lung-cancer screening in the NELSON trial, ribociclib and fulvestrant in metastatic breast cancer, vitamin D in pregnancy and asthma, treatment thresholds for neonatal hypoglycemia, and CAR-NK cells in anti-CD19 lymphoid tumors; a review article on placebo and nocebo effects; a Clinical Problem-Solving describing a rapid change in pressure; and Perspective articles on altruism in Extremis, on abuses of FDA regulatory procedures, and on joining forces against delirium.
Featuring articles on lung-cancer screening in the NELSON trial, ribociclib and fulvestrant in metastatic breast cancer, vitamin D in pregnancy and asthma, treatment thresholds for neonatal hypoglycemia, and CAR-NK cells in anti-CD19 lymphoid tumors; a review article on placebo and nocebo effects; a Clinical Problem-Solving describing a rapid change in pressure; and Perspective articles on altruism in Extremis, on abuses of FDA regulatory procedures, and on joining forces against delirium.
 Listen to a chat with Julia Adler-Milstein, the author of an editorial that comments on a recent Annals of Internal Medicine study detailing the amount of time clinicians typically spend hunched over their EHRs during a patient visit.
Listen to a chat with Julia Adler-Milstein, the author of an editorial that comments on a recent Annals of Internal Medicine study detailing the amount of time clinicians typically spend hunched over their EHRs during a patient visit.





 Medicare negotiation of prescription-drug prices would bring U.S. government policies in line with those of other high-income countries, and the idea is popular with both the public and policy analysts. But it would represent a sea change for pharmaceutical firms, which will maintain that any threat to their pricing power will slow innovation.
Medicare negotiation of prescription-drug prices would bring U.S. government policies in line with those of other high-income countries, and the idea is popular with both the public and policy analysts. But it would represent a sea change for pharmaceutical firms, which will maintain that any threat to their pricing power will slow innovation.