
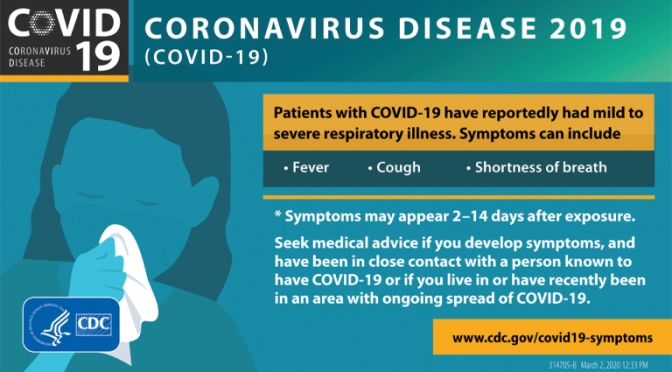
 Chloroquine was shown in 2004 to be active in vitro against SARS coronavirus but is of unproven efficacy and safety in patients infected with SARS-CoV-2. The drug’s potential benefits and risks for COVID-19 patients, without and with azithromycin, is discussed by Dr. David Juurlink, head of the Division of Clinical Pharmacology and Toxicology at Sunnybrook Health Sciences Centre in Toronto.
Chloroquine was shown in 2004 to be active in vitro against SARS coronavirus but is of unproven efficacy and safety in patients infected with SARS-CoV-2. The drug’s potential benefits and risks for COVID-19 patients, without and with azithromycin, is discussed by Dr. David Juurlink, head of the Division of Clinical Pharmacology and Toxicology at Sunnybrook Health Sciences Centre in Toronto.
From Wall Street Journal article:
Our experience suggests that hydroxychloroquine, with or without a Z-Pak, should be a first-line treatment. Unfortunately, there is already a shortage of hydroxychloroquine. The federal government should immediately contract with generic manufacturers to ramp up production. Any stockpiles should be released.
As a matter of clinical practice, hydroxychloroquine should be given early to patients who test positive, and perhaps if Covid-19 is presumed—in the case of ill household contacts, for instance. It may be especially useful to treat mild cases and young patients, which would significantly decrease viral transmission and, as they say, “flatten the curve.”


 In this Podcast Extra, we hear from epidemiologists, genomicists and social scientists about how they’re working to tackle the coronavirus and what they’ve learned so far.
In this Podcast Extra, we hear from epidemiologists, genomicists and social scientists about how they’re working to tackle the coronavirus and what they’ve learned so far.

 Drug Pricing Theme Issue: Is Pharma Earning Too Much?, R&D Costs Required to Bring a New Drug to Market, Probiotic Safety, and more
Drug Pricing Theme Issue: Is Pharma Earning Too Much?, R&D Costs Required to Bring a New Drug to Market, Probiotic Safety, and more
 “Studies with financial links to the indoor tanning industry were much more likely to discuss perceived benefits of indoor tanning and to downplay the harms,” said
“Studies with financial links to the indoor tanning industry were much more likely to discuss perceived benefits of indoor tanning and to downplay the harms,” said  In 2012, Eleni Linos, professor of dermatology at Stanford university, published a systematic review and meta-analysis of the link between non-melanoma cancer and sun-beds. That bit of pretty standard research, and a particular rapid response to it, has kicked of years of work – and in this podcast I talk to Eleni and her colleagues Stanton…
In 2012, Eleni Linos, professor of dermatology at Stanford university, published a systematic review and meta-analysis of the link between non-melanoma cancer and sun-beds. That bit of pretty standard research, and a particular rapid response to it, has kicked of years of work – and in this podcast I talk to Eleni and her colleagues Stanton…
 Intermittent fasting has salutary effects. Listen how Dr. Mark P. Mattson, co-author of a recent NEJM review on the topic, assesses the practice — and how he’s managed to skip breakfast for the past 30 years or so.
Intermittent fasting has salutary effects. Listen how Dr. Mark P. Mattson, co-author of a recent NEJM review on the topic, assesses the practice — and how he’s managed to skip breakfast for the past 30 years or so.

 In people with Type 1 diabetes, the pancreas can’t make insulin. Those with the condition require several doses of insulin a day and spent $5,705 per person on it in 2016, an increase of $2,841, or 99%, per person since 2012, according to the nonprofit
In people with Type 1 diabetes, the pancreas can’t make insulin. Those with the condition require several doses of insulin a day and spent $5,705 per person on it in 2016, an increase of $2,841, or 99%, per person since 2012, according to the nonprofit  Costs continue to rise, so much so that almost half of people with diabetes have temporarily skipped taking their insulin, according to a 2018 survey by UpWell Health, a Salt Lake City company that provides home delivery of medications and supplies for chronic conditions.
Costs continue to rise, so much so that almost half of people with diabetes have temporarily skipped taking their insulin, according to a 2018 survey by UpWell Health, a Salt Lake City company that provides home delivery of medications and supplies for chronic conditions.
 In a WTOP-FM interview, Health Affairs Editor-In-Chief Alan Weil assesses how consumers may (or may not) benefit from two long-anticipated rules, recently unveiled by the Trump Administration, that increase price transparency for both hospitals and insurers.
In a WTOP-FM interview, Health Affairs Editor-In-Chief Alan Weil assesses how consumers may (or may not) benefit from two long-anticipated rules, recently unveiled by the Trump Administration, that increase price transparency for both hospitals and insurers.