Depression is one of the most common and most debilitating mental health disorders, affecting some 17 million adults in the US. It also continues to be a misunderstood, often hard-to-treat illness. Researchers have worked for decades to better understand the neurobiology underpinning depression.
For patients with severe, treatment-resistant depression, spending months or even years searching for good treatments can be totally disabling. The prevailing hypothesis for years was that depression was regulated by the neurotransmitter’s serotonin and norepinephrine.
Eventually, data began to suggest that maybe something much larger and more global was involved in the brain to account for depression, which led researchers to begin working with glutamate and GABA, the most abundant neurotransmitters in the brain. These chemicals are involved in neuroplasticity – the brain’s ability to adapt to change and protect itself against stressful events.
Neuroplasticity is a physical thing, too: it manifests itself “in terms of synapses, how these neurons are actually touching each other and communicating with each other,” explains Gerard Sanacora, PhD, MD, Director of the Yale Depression Research Program. “And we know that in depression, the number and strength of these interconnections decreases,” says Rachel Katz, MD, a professor of Clinical Psychiatry at Yale.
Ketamine – originally developed and still used as an anesthetic – works on those two neurotransmitters and was discovered to have rapid antidepressant effects. Some experience an improvement in symptoms in 24 hours or less. “We think that one of the things that Ketamine does, that helps to explain its antidepressant effects, is help the brain to regrow the synapses, the connections between nerve cells,” says John Krystal, MD, Chair of the Department of Psychiatry at Yale.








 We tested the hypothesis that apathy, but not depression, is associated with dementia in patients with SVD. We found that higher baseline apathy, as well as increasing apathy over time, were associated with an increased dementia risk. In contrast, neither baseline depression or change in depression was associated with dementia. The relationship between apathy and dementia remained after controlling for other well-established risk factors including age, education and cognition. Finally, adding apathy to models predicting dementia improved model fit. These results suggest that apathy may be a prodromal symptom of dementia in patients with SVD.
We tested the hypothesis that apathy, but not depression, is associated with dementia in patients with SVD. We found that higher baseline apathy, as well as increasing apathy over time, were associated with an increased dementia risk. In contrast, neither baseline depression or change in depression was associated with dementia. The relationship between apathy and dementia remained after controlling for other well-established risk factors including age, education and cognition. Finally, adding apathy to models predicting dementia improved model fit. These results suggest that apathy may be a prodromal symptom of dementia in patients with SVD.
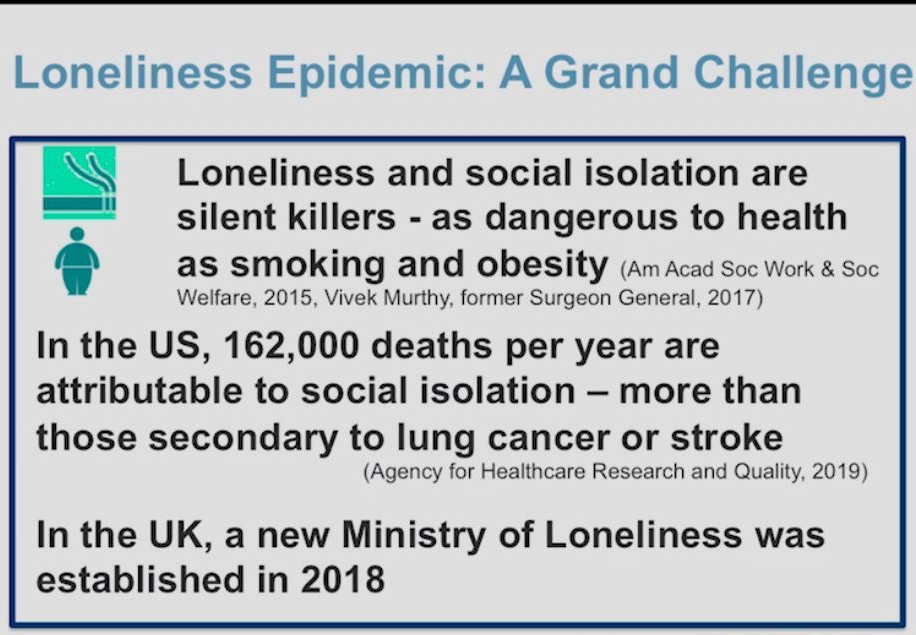 As societal stresses have increased, loneliness and social isolation have become silent killers. Dilip Jeste, MD, a geriatric neuropsychiatrist who specializes in successful aging, explains how loneliness has become an epidemic, the risk factors, helpful interventions, and how we can harness wisdom for compassion, self regulation, and more.
As societal stresses have increased, loneliness and social isolation have become silent killers. Dilip Jeste, MD, a geriatric neuropsychiatrist who specializes in successful aging, explains how loneliness has become an epidemic, the risk factors, helpful interventions, and how we can harness wisdom for compassion, self regulation, and more.

 He wondered whether lithium could have the same tranquillizing effect on his patients. After trying it out on himself to establish a safe dose, Cade began treating ten people with mania. In September 1949, he reported fast and dramatic improvements in all of them in the Medical Journal of Australia (
He wondered whether lithium could have the same tranquillizing effect on his patients. After trying it out on himself to establish a safe dose, Cade began treating ten people with mania. In September 1949, he reported fast and dramatic improvements in all of them in the Medical Journal of Australia (