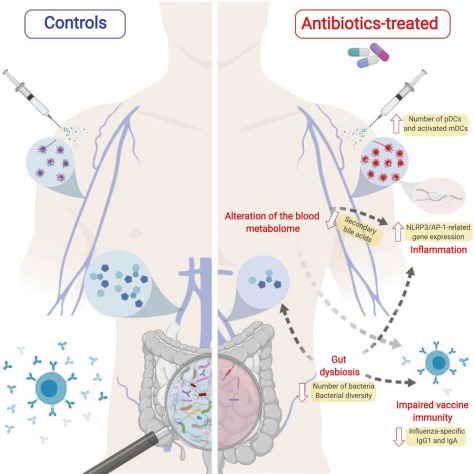
 More than 2.8 million antibiotic-resistant infections occur in the United States each year, and more than 35,000 people die as a result. In addition, nearly 223,900 people in the United States required hospital care for C. difficile and at least 12,800 people died in 2017.
More than 2.8 million antibiotic-resistant infections occur in the United States each year, and more than 35,000 people die as a result. In addition, nearly 223,900 people in the United States required hospital care for C. difficile and at least 12,800 people died in 2017.
Germs continue to spread and develop new types of resistance, and progress may be undermined by some community-associated infections that are on the rise. More action is needed to address antibiotic resistance. While the development of new treatments is one of these key actions, such investments must be coupled with dedicated efforts toward preventing infections in the first place, slowing the development of resistance through better antibiotic use, and stopping the spread of resistance when it does develop to protect American lives now and in the future.
CDC’s Antibiotic Resistance Threats in the United States, 2019 (2019 AR Threats Report) includes updated national death and infection estimates that underscore the continued threat of antibiotic resistance in the United States. New CDC data show that while the burden of antibiotic-resistance threats in the United States was greater than initially understood, deaths are decreasing since the 2013 report. This suggests that U.S. efforts—preventing infections, stopping spread of bacteria and fungi, and improving use of antibiotics in humans, animals, and the environment—are working, especially in hospitals. Vaccination, where possible, has also shown to be an effective tool of preventing infections, including those that can be resistant, in the community.
To read the report: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf



 “This study identifies a new molecular connection between exercise and inflammation that takes place in the bone marrow and highlights a previously unappreciated role of leptin in exercise-mediated cardiovascular protection,” said Michelle Olive, program officer at the National Heart, Lung, and Blood Institute Division of Cardiovascular Sciences. “This work adds a new piece to the puzzle of how sedentary lifestyles affect cardiovascular health and underscores the importance of following physical-activity guidelines.”
“This study identifies a new molecular connection between exercise and inflammation that takes place in the bone marrow and highlights a previously unappreciated role of leptin in exercise-mediated cardiovascular protection,” said Michelle Olive, program officer at the National Heart, Lung, and Blood Institute Division of Cardiovascular Sciences. “This work adds a new piece to the puzzle of how sedentary lifestyles affect cardiovascular health and underscores the importance of following physical-activity guidelines.”
 The current study points to the role of norepinephrine, a neurotransmitter that signals arousal and stress in the central nervous system. This chemical is present in low levels in the brain while we sleep, but when production ramps up it arouses our nerve cells, causing us to wake up and become alert. The study showed that norepinephrine also acts on a specific receptor, the beta2 adrenergic receptor, which is expressed at high levels in microglia. When this chemical is present in the brain, the microglia slip into a sort of hibernation.
The current study points to the role of norepinephrine, a neurotransmitter that signals arousal and stress in the central nervous system. This chemical is present in low levels in the brain while we sleep, but when production ramps up it arouses our nerve cells, causing us to wake up and become alert. The study showed that norepinephrine also acts on a specific receptor, the beta2 adrenergic receptor, which is expressed at high levels in microglia. When this chemical is present in the brain, the microglia slip into a sort of hibernation.
 “As a result, today’s epidemic of physical inactivity in conjunction with highly processed, high-sodium diets contributes to thicker, stiffer hearts that compromise the heart’s ability to cope with endurance physical activity, and importantly this may start to occur prior to increases in resting blood pressure,” explains Shave.
“As a result, today’s epidemic of physical inactivity in conjunction with highly processed, high-sodium diets contributes to thicker, stiffer hearts that compromise the heart’s ability to cope with endurance physical activity, and importantly this may start to occur prior to increases in resting blood pressure,” explains Shave. …a new
…a new 
 There may be no easy fix for the loneliness epidemic plaguing the nation, but helping people cope with hearing loss could be one key to tackling this complex problem. Hearing loss affects 1 of every 5 people and is strongly linked to loneliness: Every decibel drop in perception in people under 70 increases the odds of becoming severely lonely by 7%,
There may be no easy fix for the loneliness epidemic plaguing the nation, but helping people cope with hearing loss could be one key to tackling this complex problem. Hearing loss affects 1 of every 5 people and is strongly linked to loneliness: Every decibel drop in perception in people under 70 increases the odds of becoming severely lonely by 7%, 
 Our findings suggest that higher adherence to a Mediterranean diet is associated with better cognitive performance, and therefore less cognitive decline, in older but not middle-aged individuals.
Our findings suggest that higher adherence to a Mediterranean diet is associated with better cognitive performance, and therefore less cognitive decline, in older but not middle-aged individuals.
 The team found 85% of people first diagnosed with dementia were diagnosed by a non-dementia specialist physician, usually a primary care doctor, and an “unspecified dementia” diagnosis was common.
The team found 85% of people first diagnosed with dementia were diagnosed by a non-dementia specialist physician, usually a primary care doctor, and an “unspecified dementia” diagnosis was common. Physical inactivity, smoking, high blood pressure, diabetes, and high cholesterol play a greater role than genetics in many young patients with heart disease, according to research presented today at ESC Congress 2019 together with the World Congress of Cardiology. The findings show that healthy behaviours should be a top priority for reducing heart disease even in those with a family history of early onset.
Physical inactivity, smoking, high blood pressure, diabetes, and high cholesterol play a greater role than genetics in many young patients with heart disease, according to research presented today at ESC Congress 2019 together with the World Congress of Cardiology. The findings show that healthy behaviours should be a top priority for reducing heart disease even in those with a family history of early onset.