“Our findings show dining out is a recipe for unhealthy eating most of the time,” said Dariush Mozaffarian, senior author and dean of the Friedman School.
At fast-food restaurants, 70 percent of the meals Americans consumed were of poor dietary quality in 2015-16, down from 75 percent in 2003-04. At full-service restaurants, about 50 percent were of poor nutritional quality, an amount that remained stable over the study period. The remainder were of intermediate nutritional quality.
BOSTON (Jan. 29, 2020, 9:00 a.m. EST)—The typical American adult gets one of every five  calories from a restaurant, but eating out is a recipe for meals of poor nutritional quality in most cases, according to a new study by researchers at the Friedman School of Nutrition Science and Policy at Tufts University.
calories from a restaurant, but eating out is a recipe for meals of poor nutritional quality in most cases, according to a new study by researchers at the Friedman School of Nutrition Science and Policy at Tufts University.

Published today in The Journal of Nutrition, the study analyzed the dietary selections of more than 35,000 U.S. adults from 2003-2016 in the National Health and Nutrition Examination Survey (NHANES) who dined at full-service (those with wait staff) or fast-food restaurants, which included pizza shops and what has become known as fast-casual. The researchers assessed nutritional quality by evaluating specific foods and nutrients in the meals, based on the American Heart Association 2020 diet score.


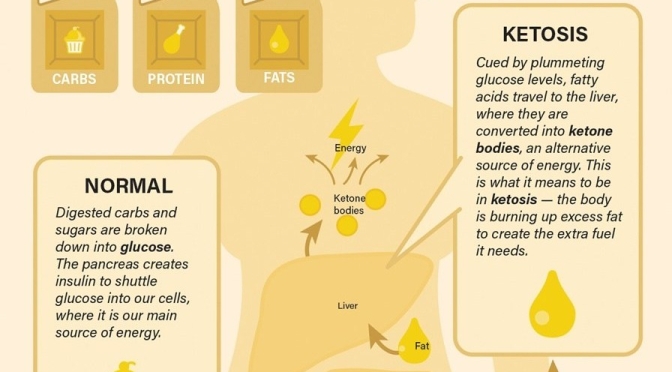
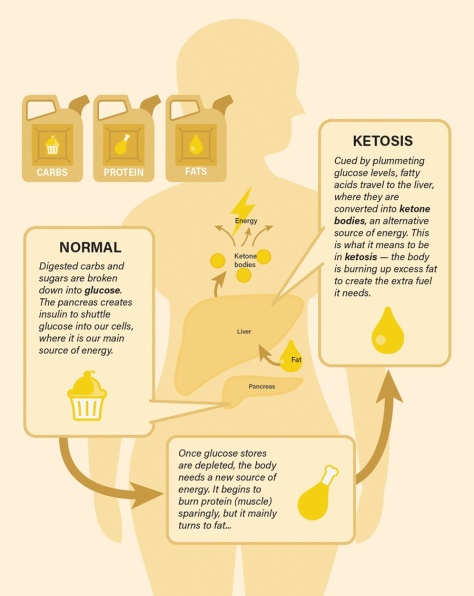
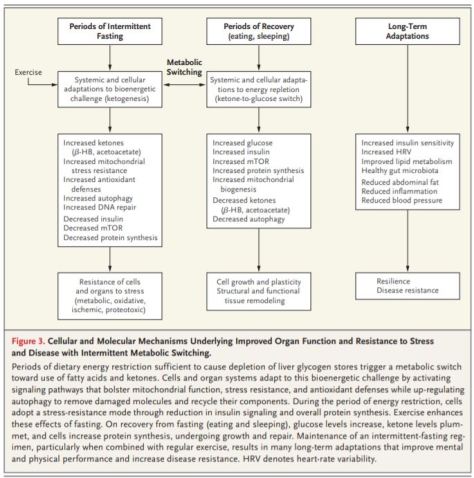
 to a paper Mattson and colleagues published in February in the experimental biology journal FASEB. In humans, fasting for 12 hours or more drops the levels of glycogen, a form of cellular glucose. Like changing to a backup gas tank, the body switches from glucose to fatty acids, a more efficient fuel. The switch generates the production of ketones, which are energy molecules that are made in the liver. “When the fats are mobilized and used to produce ketones, we think that is a key factor in accruing the health benefits,” says Mattson.
to a paper Mattson and colleagues published in February in the experimental biology journal FASEB. In humans, fasting for 12 hours or more drops the levels of glycogen, a form of cellular glucose. Like changing to a backup gas tank, the body switches from glucose to fatty acids, a more efficient fuel. The switch generates the production of ketones, which are energy molecules that are made in the liver. “When the fats are mobilized and used to produce ketones, we think that is a key factor in accruing the health benefits,” says Mattson.
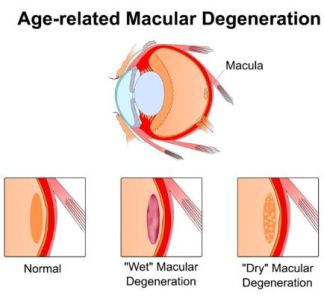 “Our work provides additional evidence that that diet matters,” Millen added. “From a public health standpoint, we can tell people that if you have early AMD, it is likely in your best interest to limit your intake of processed meat, fried food, refined grains, and high-fat dairy to preserve your vision over time.”
“Our work provides additional evidence that that diet matters,” Millen added. “From a public health standpoint, we can tell people that if you have early AMD, it is likely in your best interest to limit your intake of processed meat, fried food, refined grains, and high-fat dairy to preserve your vision over time.”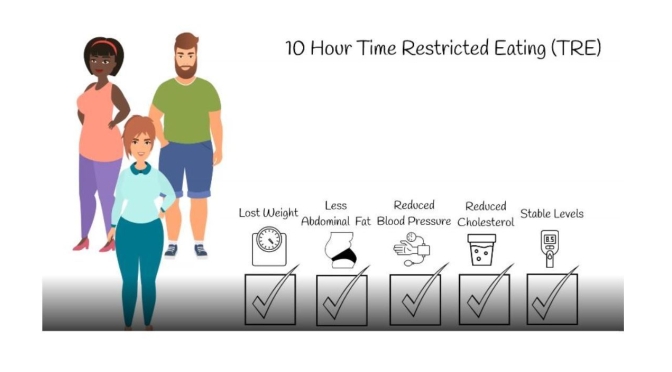
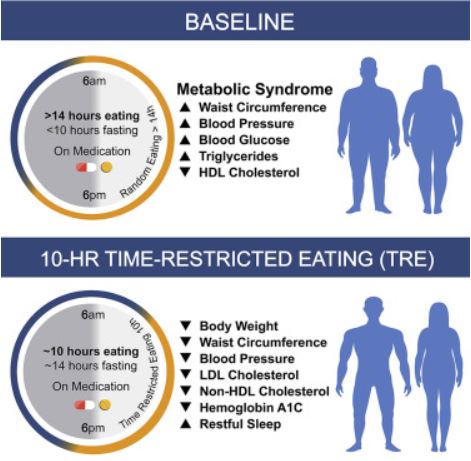
 Ten-hour time-restricted eating (TRE) limits daily dietary intake to a consistent 10-h window, creating a 14-h nightly fast. Researchers studied whether TRE for 12 weeks in people with metabolic syndrome receiving standard medical care (including medications to lower cholesterol and blood pressure) improves markers of health. TRE led to weight loss, healthier body composition (including decreased waist circumference), lower blood pressure and levels of cardiovascular disease-promoting lipids (i.e., “bad cholesterol” levels), and more restful sleep. TRE could be an effective dietary intervention to help those with metabolic syndrome.
Ten-hour time-restricted eating (TRE) limits daily dietary intake to a consistent 10-h window, creating a 14-h nightly fast. Researchers studied whether TRE for 12 weeks in people with metabolic syndrome receiving standard medical care (including medications to lower cholesterol and blood pressure) improves markers of health. TRE led to weight loss, healthier body composition (including decreased waist circumference), lower blood pressure and levels of cardiovascular disease-promoting lipids (i.e., “bad cholesterol” levels), and more restful sleep. TRE could be an effective dietary intervention to help those with metabolic syndrome.