At HMS, Maofu Liao is establishing a new research pipeline to improve the process of antibiotic development https://t.co/4G2nyGKzWQ
— Harvard Medical School (@harvardmed) November 4, 2021
Tag Archives: Antibiotic Resistance
Analysis: Multiresistant Bacteria That Outsmart Antibiotics (Video)
Antimicrobial resistance is one of the greatest medical challenges of our time. Among the causes are industrial livestock farming, poor hygiene in hospitals, and the misuse of antibiotics. This documentary looks at approaches to fighting multiresistant strains of bacteria.
Each year 33,000 people in Europe die after becoming infected with bacteria that are resistant to antibiotics. Hygiene specialist Dr. Ron Hendrix has been working for years to prevent outbreaks of infectious disease in hospitals. Dr. Hendrix says that he and other experts in the Netherlands recognized early on that they’d have to fight the spread of bacteria just as actively as they would the actual infection.
Hendrix has convinced a number of German hospitals to re-open their diagnostic laboratories, as well. In the early 2000s, many of these labs had been shut down as a cost-cutting measure. And farmers in Denmark voluntarily chose to sharply reduce their use of antibiotics, after evidence showed that intensive livestock farming caused multiresistant bacteria to multiply.
Infectious disease specialist Dr. Patrick Soentjens was able to convince Belgium’s health ministry to allow the use of “phages” to treat stubborn antimicrobial resistant pathogens. Phages are special viruses that kill bacteria. Dr. Soentjens is certain that this well-known, but largely forgotten option could save many lives. Belgium has become the first western European country where phages have been officially recognized as a legitimate medical treatment.
TOP JOURNALS: RESEARCH HIGHLIGHTS FROM SCIENCE MAGAZINE (NOV 20, 2020)
Study: “Probiotic Drink” Developed That Thwarts Antibiotic Resistance
From a Genetic Engineering & Biotechnology News online article:
 “We were able to show that if you can stop the plasmid from replicating, then most of the bacteria lose the plasmid as the bacteria grow and divide. This means that infections that might otherwise be hard to control, even with the most powerful antibiotics available, are more likely to be treatable with standard antibiotics.”
“We were able to show that if you can stop the plasmid from replicating, then most of the bacteria lose the plasmid as the bacteria grow and divide. This means that infections that might otherwise be hard to control, even with the most powerful antibiotics available, are more likely to be treatable with standard antibiotics.”
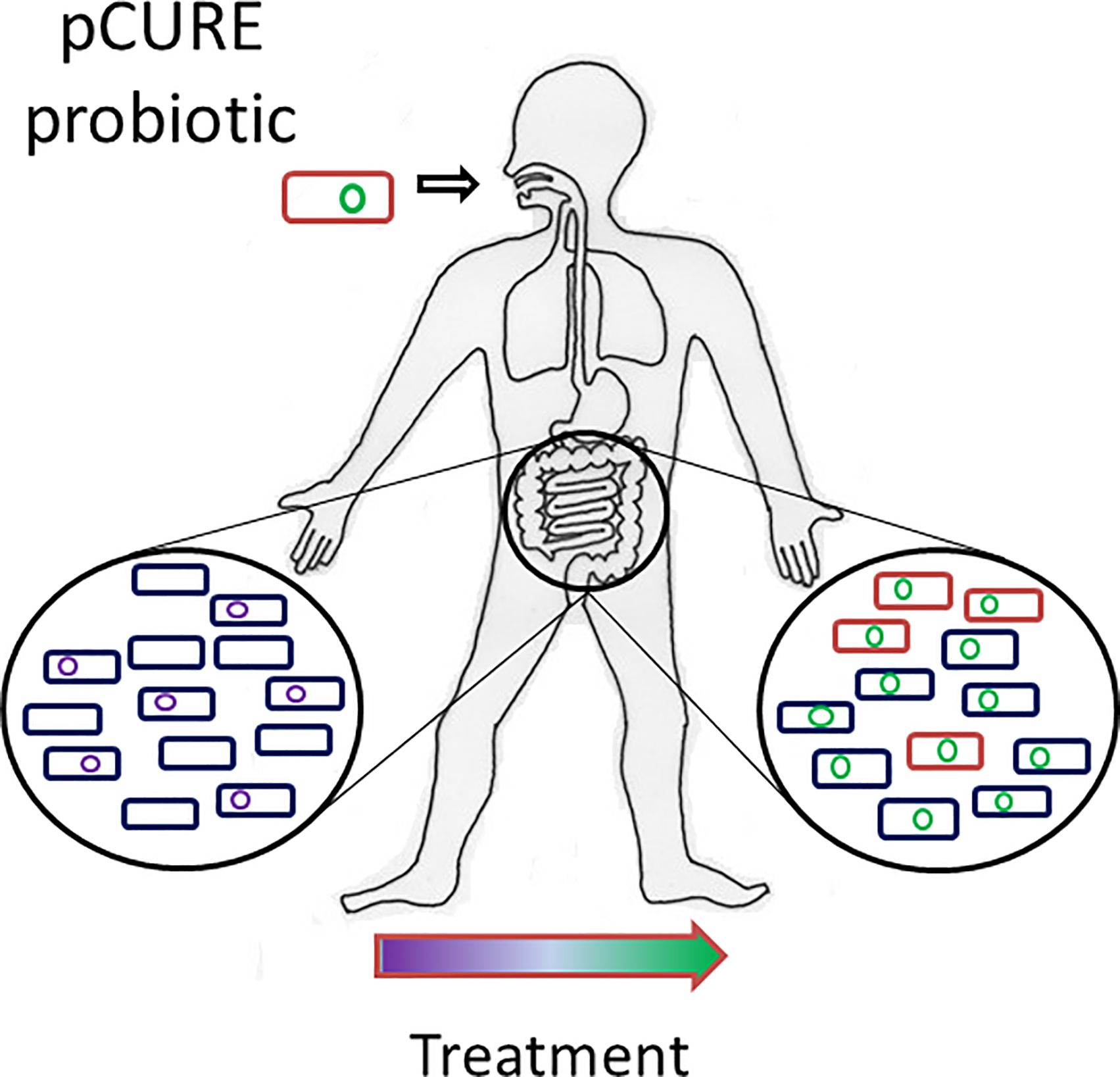
Researchers headed by a team at the University of Birmingham in the U.K. have developed a probiotic drink containing genetic elements that are designed to thwart antimicrobial resistance (AMR) in gut bacteria at the genetic level. The drink targets small DNA elements called plasmids that carry antibiotic resistance genes, and which are able to replicate independently and spread between bacteria. By preventing these plasmids from replicating, the antibiotic resistance genes are displaced, effectively resensitizing the bacteria to antibiotics.
New Health Studies: 43% Of Americans Prescribed Antibiotics Improperly
From a British Medical Journal (BMJ) online article:
 …primary care providers (general practice, paediatrics, and internal medicine) performed the best, giving a considerably lower percentage of antibiotic prescriptions without a documented indication (12%) than other specialists such as gynaecologists and urologists, who commonly prescribed antibiotics (24%), as well as those in all other specialties (29%).
…primary care providers (general practice, paediatrics, and internal medicine) performed the best, giving a considerably lower percentage of antibiotic prescriptions without a documented indication (12%) than other specialists such as gynaecologists and urologists, who commonly prescribed antibiotics (24%), as well as those in all other specialties (29%).
As many as two in five antibiotic prescriptions (43%) provided in outpatient settings in the US could be inappropriate, a study published by The BMJ has found.1
Researchers from Oregon, USA, looked at prescriptions in ambulatory settings such as primary care and found that a quarter (25%) were deemed to be inappropriate, while a further 18% did not have an indication.
To read more: https://www.bmj.com/content/367/bmj.l6961
Health Reports: CDC Finds That 35,000 Americans Die Of Antibiotic-Resistant Infections Each Year
 More than 2.8 million antibiotic-resistant infections occur in the United States each year, and more than 35,000 people die as a result. In addition, nearly 223,900 people in the United States required hospital care for C. difficile and at least 12,800 people died in 2017.
More than 2.8 million antibiotic-resistant infections occur in the United States each year, and more than 35,000 people die as a result. In addition, nearly 223,900 people in the United States required hospital care for C. difficile and at least 12,800 people died in 2017.
Germs continue to spread and develop new types of resistance, and progress may be undermined by some community-associated infections that are on the rise. More action is needed to address antibiotic resistance. While the development of new treatments is one of these key actions, such investments must be coupled with dedicated efforts toward preventing infections in the first place, slowing the development of resistance through better antibiotic use, and stopping the spread of resistance when it does develop to protect American lives now and in the future.
CDC’s Antibiotic Resistance Threats in the United States, 2019 (2019 AR Threats Report) includes updated national death and infection estimates that underscore the continued threat of antibiotic resistance in the United States. New CDC data show that while the burden of antibiotic-resistance threats in the United States was greater than initially understood, deaths are decreasing since the 2013 report. This suggests that U.S. efforts—preventing infections, stopping spread of bacteria and fungi, and improving use of antibiotics in humans, animals, and the environment—are working, especially in hospitals. Vaccination, where possible, has also shown to be an effective tool of preventing infections, including those that can be resistant, in the community.
To read the report: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf
Health: Asymptomatic Bacteriuria Diagnosis In Older Patients Should Not Require Antibiotics
From a New York Times online article:
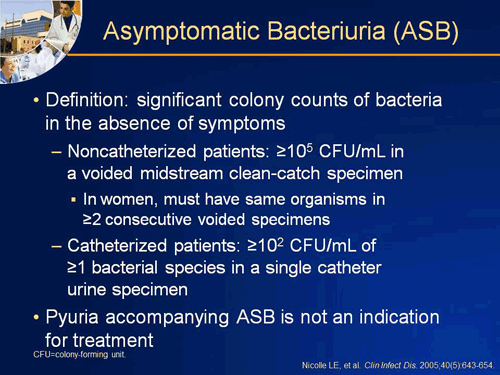 At Dr. Soong’s hospital, withholding the results of urine cultures, unless doctors actually called the microbiology lab to request them, reduced prescriptions for asymptomatic bacteriuria to 12 percent from 48 percent of non-catheterized patients, with no loss of safety.
At Dr. Soong’s hospital, withholding the results of urine cultures, unless doctors actually called the microbiology lab to request them, reduced prescriptions for asymptomatic bacteriuria to 12 percent from 48 percent of non-catheterized patients, with no loss of safety.
“The extra step of having the clinician call eliminated a lot of frivolous testing,” Dr. Soong said.
In patients who have none of the typical symptoms of a urinary tract infection — no painful or frequent urination, no blood in the urine, no fever or lower abdominal tenderness — lab results detecting bacteria in the urine don’t indicate infection and thus shouldn’t trigger treatment.
Older people, and nursing home residents in particular, often have urinary systems colonized by bacteria; they will have a positive urine test almost every time, but they’re not sick.
To read more: https://www.nytimes.com/2019/10/14/health/urine-tests-elderly.html
Long-Term Care: A Highly Contagious, Drug-Resistant “Fatal Fungus” Spreads In Nursing Homes
From a New York Times online article:
 Scientific research on nursing homes and drug resistance is sparse, but some recent studies offer evidence of the problem. A study published in June in the Journal of Clinical Infectious Diseases found that patients and residents in long-term care settings have alarmingly high rates of drug-resistant colonization, which means they carry the germs on their skin or in their bodies, usually without knowing it, and can pass them invisibly to staff members, relatives or other patients. Elderly or severely ill people with weakened immune systems who carry the germ are at high risk of becoming infected.
Scientific research on nursing homes and drug resistance is sparse, but some recent studies offer evidence of the problem. A study published in June in the Journal of Clinical Infectious Diseases found that patients and residents in long-term care settings have alarmingly high rates of drug-resistant colonization, which means they carry the germs on their skin or in their bodies, usually without knowing it, and can pass them invisibly to staff members, relatives or other patients. Elderly or severely ill people with weakened immune systems who carry the germ are at high risk of becoming infected.
Maria Davila lay mute in a nursing home bed, an anguished expression fixed to her face, as her husband stroked her withered hand. Ms. Davila, 65, suffers from a long list of ailments — respiratory failure, kidney disease, high blood pressure, an irregular heartbeat — and is kept alive by a gently beeping ventilator and a feeding tube.
Doctors recently added another diagnosis to her medical chart: Candida auris, a highly contagious, drug-resistant fungus that has infected nearly 800 people since it arrived in the United States four years ago, with half of patients dying within 90 days.
To read more: www.nytimes.com/2019/09/11/health/nursing-homes-fungus.html?action=click&module=News&pgtype=Homepage
Top Science Podcasts: Persistent Antibiotic Resistance And Modeling Hot Cities (Nature)
 Researchers have identified how Salmonella ‘persister’ cells can spread antibiotic resistance genes in mice intestines.
Researchers have identified how Salmonella ‘persister’ cells can spread antibiotic resistance genes in mice intestines.
Cities are generally hotter than their surroundings, but what are the causes of these ‘heat islands’?
In this episode:
00:46 Antibiotic resistance reservoirs
Researchers have identified how Salmonella ‘persister’ cells can spread antibiotic resistance genes in mice intestines. Research article: Bakkeren et al.
08:12 Research Highlights
Bright barn owls stun prey, and the evolution of dog brains. Research Highlight: Zip-lining owls reveal what really scares their prey; Research Highlight: A dog’s breed is a window onto its brain
10:13 Urban heating
Cities are generally hotter than their surroundings, but what are the causes of these ‘heat islands’? Research Article: Manoli et al.
16:54 News Chat
A cryptic Russian radiation spike, and India’s moon mission gets closer to touchdown. News: How nuclear scientists are decoding Russia’s mystery explosion; News: ‘The most terrifying moments’: India counts down to risky Moon landing
Drug Studies: Ibuprofen & Anti-Inflammatories “Enhance Spread Of Antibiotic Resistance
From a BioRxiv.com online news release:
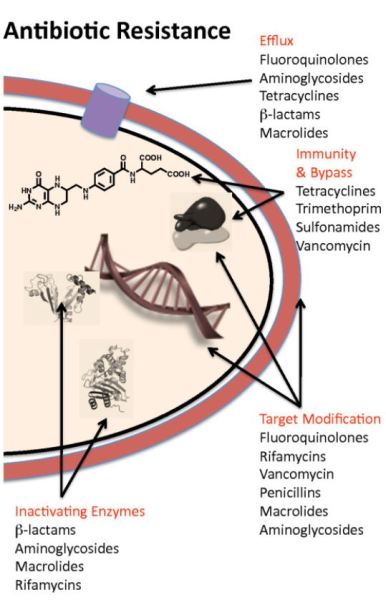 Antibiotic resistance is a global threat for public health. It is widely acknowledged that antibiotics at sub-inhibitory concentrations are important in disseminating antibiotic resistance via horizontal gene transfer. While there is high use of non-antibiotic human-targeted pharmaceuticals in our societies, the potential contribution of these on the spread of antibiotic resistance has been overlooked so far. Here, we report that commonly consumed non-antibiotic pharmaceuticals, including nonsteroidal anti-inflammatories (ibuprofen, naproxen, diclofenac), a lipid-lowering drug (gemfibrozil), and a β-blocker (propanolol), at clinically and environmentally relevant concentrations, significantly accelerated the conjugation of plasmid-borne antibiotic resistance genes.
Antibiotic resistance is a global threat for public health. It is widely acknowledged that antibiotics at sub-inhibitory concentrations are important in disseminating antibiotic resistance via horizontal gene transfer. While there is high use of non-antibiotic human-targeted pharmaceuticals in our societies, the potential contribution of these on the spread of antibiotic resistance has been overlooked so far. Here, we report that commonly consumed non-antibiotic pharmaceuticals, including nonsteroidal anti-inflammatories (ibuprofen, naproxen, diclofenac), a lipid-lowering drug (gemfibrozil), and a β-blocker (propanolol), at clinically and environmentally relevant concentrations, significantly accelerated the conjugation of plasmid-borne antibiotic resistance genes.
To read more click on following link: https://www.biorxiv.org/content/10.1101/724500v1.full