From a Wall Street Journal article (April 18 2020)
 A physical therapist based in Santa Barbara, Calif., Ms. Godges is used to seeing injuries that result when swimmers start training on land. “We are great at cardio, but we aren’t used to pounding our joints. Gravity is not forgiving. We need to give our bodies time to adapt.”
A physical therapist based in Santa Barbara, Calif., Ms. Godges is used to seeing injuries that result when swimmers start training on land. “We are great at cardio, but we aren’t used to pounding our joints. Gravity is not forgiving. We need to give our bodies time to adapt.”
With pools closed over concerns about coronavirus transmission, Arlette Godges is adapting to being a fish on land.
The 55-year-old U.S. Masters swimmer was in the pool five days a week training for the UANA Pan American Masters Championships in Medellín, Colombia. The June competition has been postponed. “I was feeling so strong,” she says. “Now I have to challenge myself with other things so I don’t become a slug and lose motivation.”


 It was all horribly familiar — a rerun of an episode 15 months earlier, when she was with her family in River Vale, N.J. Back then, the burning pressure sent her to the emergency department, and she was told the same thing: She was having a heart attack. Immediately the cardiologist looked for blockages in the coronary arteries, which feed blood and oxygen to the hardworking muscles of her heart. That was the cause of most heart attacks. But they found no blockage.
It was all horribly familiar — a rerun of an episode 15 months earlier, when she was with her family in River Vale, N.J. Back then, the burning pressure sent her to the emergency department, and she was told the same thing: She was having a heart attack. Immediately the cardiologist looked for blockages in the coronary arteries, which feed blood and oxygen to the hardworking muscles of her heart. That was the cause of most heart attacks. But they found no blockage. Indeed, that was the clue that led the rheumatologist to a likely diagnosis: Behcet’s disease. It’s an unusual inflammatory disorder characterized by joint pains, muscle pains and recurrent ulcers in mucus membranes throughout the body. Almost any part of the body can be involved — the eyes, the nose and lungs, the brain, the blood vessels, even the heart. Behcet’s was named after a Turkish dermatologist who in 1937 described a triad of clinical findings including canker sores (medically known as aphthous ulcers), genital ulcers and an inflammatory condition of the eye.
Indeed, that was the clue that led the rheumatologist to a likely diagnosis: Behcet’s disease. It’s an unusual inflammatory disorder characterized by joint pains, muscle pains and recurrent ulcers in mucus membranes throughout the body. Almost any part of the body can be involved — the eyes, the nose and lungs, the brain, the blood vessels, even the heart. Behcet’s was named after a Turkish dermatologist who in 1937 described a triad of clinical findings including canker sores (medically known as aphthous ulcers), genital ulcers and an inflammatory condition of the eye.
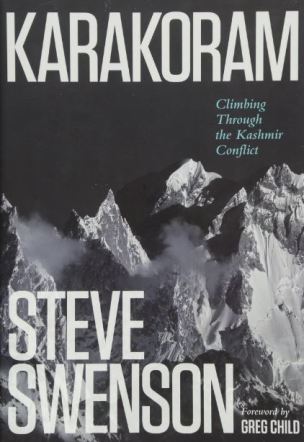 In the spring and summer, he trained two to four hours a day, six days a week, running daily and carrying 60 pounds of water up a 4,000-foot peak near his home in Seattle twice a week. “All the research has shown that 80 percent of training for alpine ascents needs to be long duration and low intensity, to build a huge foundation of endurance,” Swenson says. “There are no shortcuts to this. There’s no thirty-minute-a-day gym workout. You have to have the discipline to put the time in.”
In the spring and summer, he trained two to four hours a day, six days a week, running daily and carrying 60 pounds of water up a 4,000-foot peak near his home in Seattle twice a week. “All the research has shown that 80 percent of training for alpine ascents needs to be long duration and low intensity, to build a huge foundation of endurance,” Swenson says. “There are no shortcuts to this. There’s no thirty-minute-a-day gym workout. You have to have the discipline to put the time in.” 
 The current study points to the role of norepinephrine, a neurotransmitter that signals arousal and stress in the central nervous system. This chemical is present in low levels in the brain while we sleep, but when production ramps up it arouses our nerve cells, causing us to wake up and become alert. The study showed that norepinephrine also acts on a specific receptor, the beta2 adrenergic receptor, which is expressed at high levels in microglia. When this chemical is present in the brain, the microglia slip into a sort of hibernation.
The current study points to the role of norepinephrine, a neurotransmitter that signals arousal and stress in the central nervous system. This chemical is present in low levels in the brain while we sleep, but when production ramps up it arouses our nerve cells, causing us to wake up and become alert. The study showed that norepinephrine also acts on a specific receptor, the beta2 adrenergic receptor, which is expressed at high levels in microglia. When this chemical is present in the brain, the microglia slip into a sort of hibernation.
 Now 63, Mr. Peterson has progressed from bike paths to rugged mountain trails and is known for his caped helmet emblazoned with his nickname, UniGeezer. Based on his GPS and bike computer, he estimates he’s logged nearly 30,000 miles, or 24 million pedal revolutions, since he started.
Now 63, Mr. Peterson has progressed from bike paths to rugged mountain trails and is known for his caped helmet emblazoned with his nickname, UniGeezer. Based on his GPS and bike computer, he estimates he’s logged nearly 30,000 miles, or 24 million pedal revolutions, since he started.
 Dr. Grace Dammann, medical director of the Pain Clinic at Laguna Honda Hospital, and seven of her colleagues talk about what does and does not work in the treatment of chronic pain. She talks as both a patient and a provider. There is also a discussion of various non-pharmacologic and complementary medicine modalities to treat pain.
Dr. Grace Dammann, medical director of the Pain Clinic at Laguna Honda Hospital, and seven of her colleagues talk about what does and does not work in the treatment of chronic pain. She talks as both a patient and a provider. There is also a discussion of various non-pharmacologic and complementary medicine modalities to treat pain.






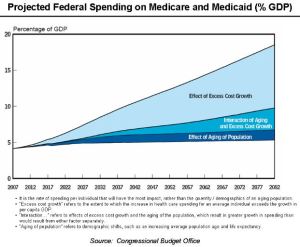 I once witnessed the care of a patient who suffered from chronic obstructive pulmonary disease, which blocks airflow to lungs and makes it difficult to breathe. Over the course of a particularly hot Texas summer, he was admitted to the hospital time and time again—racking up more than $60,000 in medical expenses. Doctors were treating his breathing problems repeatedly, but they did not understand why the patient continued to have trouble.
I once witnessed the care of a patient who suffered from chronic obstructive pulmonary disease, which blocks airflow to lungs and makes it difficult to breathe. Over the course of a particularly hot Texas summer, he was admitted to the hospital time and time again—racking up more than $60,000 in medical expenses. Doctors were treating his breathing problems repeatedly, but they did not understand why the patient continued to have trouble. Thin, soft electronic systems that stick onto skin are beginning to transform health care. Millions of early versions
Thin, soft electronic systems that stick onto skin are beginning to transform health care. Millions of early versions