From the Wall Street Journal (June 8, 2020):
“We have to operate a hospital within a hospital, taking care of the needs for patients who have had strokes or a newborn delivery or need surgery while dealing with an otherwise healthy 35-year-old who picked up Covid-19 at a social event,” says James Linder, chief executive of Nebraska Medicine…
 For instance, more hospitals are remotely triaging and registering patients before they even arrive. Clinicians can consult with patients from their home via telemedicine to help determine how sick they are and if they need to come to the ER at all. From there, admissions are made with as little contact with staff or other patients as possible.
For instance, more hospitals are remotely triaging and registering patients before they even arrive. Clinicians can consult with patients from their home via telemedicine to help determine how sick they are and if they need to come to the ER at all. From there, admissions are made with as little contact with staff or other patients as possible.
Hospitals are rethinking how they operate in light of the Covid-19 pandemic—and preparing for a future where such crises may become a grim fact of life.
 With the potential for resurgences of the coronavirus, and some scientists warning about outbreaks of other infectious diseases, hospitals don’t want to be caught flat-footed again. So, more of them are turning to new protocols and new technology to overhaul standard operating procedure, from the time patients show up at an emergency room through admission, treatment and discharge.
With the potential for resurgences of the coronavirus, and some scientists warning about outbreaks of other infectious diseases, hospitals don’t want to be caught flat-footed again. So, more of them are turning to new protocols and new technology to overhaul standard operating procedure, from the time patients show up at an emergency room through admission, treatment and discharge.



 Cardiovascular consults are way down. Is the threat of COVID-19 infection scaring people away from ED’s?
Cardiovascular consults are way down. Is the threat of COVID-19 infection scaring people away from ED’s?
 Facing shortages of critical equipment, medical workers must make life-or-death decisions about who receives care. WSJ’s Joe Palazzolo reports from an emergency room that’s running short on ventilators, and Chris Weaver explains the plans hospitals are putting in place to decide who gets them.
Facing shortages of critical equipment, medical workers must make life-or-death decisions about who receives care. WSJ’s Joe Palazzolo reports from an emergency room that’s running short on ventilators, and Chris Weaver explains the plans hospitals are putting in place to decide who gets them. 
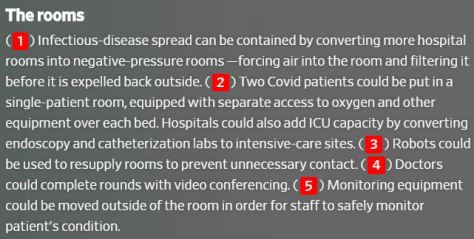
 Produced by WIRED Brand Lab with American Institute of Architects | How can design transform emergency rooms from one of the most stressful and chaotic places into a place of healing? Dr. Bon Ku and architect Billie Faircloth, AIA, break down the science behind designing a better work environment for hospitals.
Produced by WIRED Brand Lab with American Institute of Architects | How can design transform emergency rooms from one of the most stressful and chaotic places into a place of healing? Dr. Bon Ku and architect Billie Faircloth, AIA, break down the science behind designing a better work environment for hospitals.
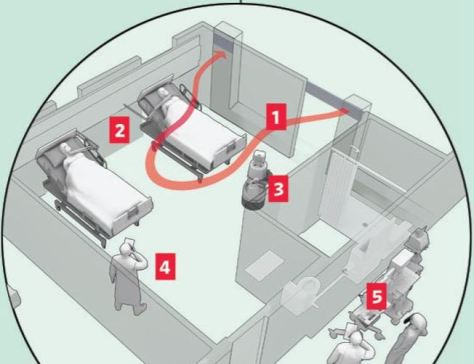
 The
The