
1. HANDS Wash them often
2. ELBOW Cough into it
3. FACE Don’t touch it
4. FEET Stay 3 ft from other people
5. FEEL sick? Stay home

If you are sick with COVID-19 or suspect you are infected with the virus that causes COVID-19, follow the steps below to help prevent the disease from spreading to people in your home and community.
Syndicated columnist Mark Shields and New York Times columnist David Brooks join Judy Woodruff to discuss the week’s political news, including the unique magnitude of the novel coronavirus pandemic, how President Trump is handling the crisis, what the government should do to reassure fearful Americans, and how the outbreak might affect the 2020 Democratic presidential primary race.
 Monocle 24 “The Urbanist” discusses the impact that quarantines can have on cities and what lessons city planners can learn when an outbreak causes borders to close. Here is a report from the ground on the changing nature of city life in Milan.
Monocle 24 “The Urbanist” discusses the impact that quarantines can have on cities and what lessons city planners can learn when an outbreak causes borders to close. Here is a report from the ground on the changing nature of city life in Milan.What happens if you overwater a plant? How does gravity actually work? And should we be cancelling mass events to contain the coronavirus?
It’s Q&A time on the show, and this week Phil Sansom is joined by a brainy panel of experts: plant biologist Nadia Radzman, particle physicist Chris Rogers, bioarchaeologist Emma Pomeroy, and virologist and Naked Scientist Chris Smith. Prepare to have your curiosity satisfied…
Dr. Matthew Binnicker oversees Mayo Clinic’s laboratory response in developing a test to detect COVID-19 in clinical samples. A process that usually takes six months to a year, was accomplished in under a month, thanks to a dedicated team working around the clock. The test should help ease the burden currently being felt at the Centers for Disease Control & Prevention and state health labs. That will also mean faster turnaround times for results. Patients can expect results within 24 hours of when samples are collected and sent to Mayo Clinic Laboratories. Initially, Dr. Binnicker says the laboratory has the capacity to run between 200-300 tests daily. Additional equipment has been ordered to double that capacity in the coming weeks.
More health and medical news on the Mayo Clinic News Network. https://newsnetwork.mayoclinic.org/
Global health officials have praised China and South Korea for the success of their efforts to contain the coronavirus. What are those countries getting right — and what can everyone else learn from them?
Guest: Donald G. McNeil Jr., a science and health reporter for The New York Times. For more information on today’s episode, visit nytimes.com/thedaily.
Background reading:
From a New England Journal of Medicine article (March 11, 2020):
 A central strategy for health care surge control is “forward triage” — the sorting of patients before they arrive in the emergency department (ED). Direct-to-consumer (or on-demand) telemedicine, a 21st-century approach to forward triage that allows patients to be efficiently screened, is both patient-centered and conducive to self-quarantine, and it protects patients, clinicians, and the community from exposure.
A central strategy for health care surge control is “forward triage” — the sorting of patients before they arrive in the emergency department (ED). Direct-to-consumer (or on-demand) telemedicine, a 21st-century approach to forward triage that allows patients to be efficiently screened, is both patient-centered and conducive to self-quarantine, and it protects patients, clinicians, and the community from exposure.
It can allow physicians and patients to communicate 24/7, using smartphones or webcam-enabled computers. Respiratory symptoms — which may be early signs of Covid-19 — are among the conditions most commonly evaluated with this approach. Health care providers can easily obtain detailed travel and exposure histories. Automated screening algorithms can be built into the intake process, and local epidemiologic information can be used to standardize screening and practice patterns across providers.
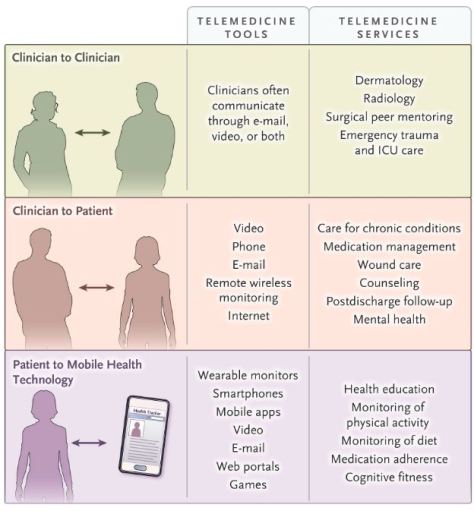
More than 50 U.S. health systems already have such programs. Jefferson Health, Mount Sinai, Kaiser Permanente, Cleveland Clinic, and Providence, for example, all leverage telehealth technology to allow clinicians to see patients who are at home. Systems lacking such programs can outsource similar services to physicians and support staff provided by Teladoc Health or American Well. At present, the major barrier to large-scale telemedical screening for SARS-CoV-2, the novel coronavirus causing Covid-19, is coordination of testing. As the availability of testing sites expands, local systems that can test appropriate patients while minimizing exposure — using dedicated office space, tents, or in-car testing — will need to be developed and integrated into telemedicine workflows.
From an MIT Technology Review article (March 11, 2020):
Here are six differences between coronavirus and the flu:
 Coronavirus appears to spread more slowly than the flu. This is probably the biggest difference between the two. The flu has a shorter incubation period (the time it takes for an infected person to show symptoms) and a shorter serial interval (or the time between successive cases). Coronavirus’s serial interval is around five to six days, while flu’s gap between cases is more like three days, the WHO says. So flu still spreads more quickly.
Coronavirus appears to spread more slowly than the flu. This is probably the biggest difference between the two. The flu has a shorter incubation period (the time it takes for an infected person to show symptoms) and a shorter serial interval (or the time between successive cases). Coronavirus’s serial interval is around five to six days, while flu’s gap between cases is more like three days, the WHO says. So flu still spreads more quickly. Don’t blame snotty kids—adults are passing coronavirus around. While kids are the primary culprits for flu transmission, this coronavirus seems to be passed between adults. That also means adults are getting hit hardest—especially those who are older and have underlying medical conditions. Experts are baffled as to why kids seem protected from the worst effects of the coronavirus, according to the Washington Post. Some say they might already have some immunity from other versions of the coronavirus that appear in the common cold; another theory is that kids’ immune systems are always on high alert and might simply be faster than adults’ in battling Covid-19.
Don’t blame snotty kids—adults are passing coronavirus around. While kids are the primary culprits for flu transmission, this coronavirus seems to be passed between adults. That also means adults are getting hit hardest—especially those who are older and have underlying medical conditions. Experts are baffled as to why kids seem protected from the worst effects of the coronavirus, according to the Washington Post. Some say they might already have some immunity from other versions of the coronavirus that appear in the common cold; another theory is that kids’ immune systems are always on high alert and might simply be faster than adults’ in battling Covid-19.From a Harvard Gazette online article (March 10, 2020):
 There’s a symptom review, there’s a travel review, and there’s an exposure review. And if the answer to any of those questions is yes, then you’re asked to not come in. And so far people have been compliant and have left. So that is a good thing.
There’s a symptom review, there’s a travel review, and there’s an exposure review. And if the answer to any of those questions is yes, then you’re asked to not come in. And so far people have been compliant and have left. So that is a good thing.
If you have a cough and a fever, if you’ve got respiratory symptoms and you’re short of breath, if you’ve traveled to a place of concern or if you may have been exposed to someone who did — especially if you’re symptomatic — then I would definitely ask, “Do I really need to visit my grandma today? Can I wait and can I Skype her? Can I do FaceTime?”
I know that’s hard for some of our older adults who aren’t technologically savvy, but maybe now is the time to get them hooked up. It really would be heartbreaking if, in wanting to do something positive for someone’s emotional or mental health, you ended up infecting them.
Harvard-affiliated Hebrew SeniorLife offers a continuum of care for 3,000 elderly people daily, with a range of services including residential assisted living, short-term rehabilitation, outpatient services, and long-term care for those with chronic illness. In a Q&A interview aimed at understanding the challenges involved, Harvard Medical School Assistant Professor Helen Chen, Hebrew SeniorLife’s chief medical officer, discussed steps the facility has taken to combat the virus and the outlook going forward.