From a Neurology.org online Journal article:
 Low and high levels of hemoglobin are associated with an increased risk of dementia, including AD, which may relate to differences in white matter integrity and cerebral perfusion.
Low and high levels of hemoglobin are associated with an increased risk of dementia, including AD, which may relate to differences in white matter integrity and cerebral perfusion.
Objective: To determine the long-term association of hemoglobin levels and anemia with risk of dementia, and explore underlying substrates on brain MRI in the general population.
Methods: Serum hemoglobin was measured in 12,305 participants without dementia of the populationbased Rotterdam Study (mean age 64.6 years, 57.7% women). We determined risk of dementia and Alzheimer disease (AD) (until 2016) in relation to hemoglobin and anemia. Among 5,267 participants without dementia with brain MRI, we assessed hemoglobin in relation to vascular brain disease, structural connectivity, and global cerebral perfusion.
To read more click on following link: https://n.neurology.org/content/neurology/early/2019/07/31/WNL.0000000000008003.full.pdf






 A blood test to detect the brain changes of early Alzheimer’s disease has moved one step closer to reality. Researchers from Washington University School of Medicine in St. Louis report that they can measure levels of the Alzheimer’s protein amyloid beta in the blood and use such levels to predict whether the protein has accumulated in the brain. The findings represent a key step toward a blood test to diagnose people on track to develop the devastating disease before symptoms arise.
A blood test to detect the brain changes of early Alzheimer’s disease has moved one step closer to reality. Researchers from Washington University School of Medicine in St. Louis report that they can measure levels of the Alzheimer’s protein amyloid beta in the blood and use such levels to predict whether the protein has accumulated in the brain. The findings represent a key step toward a blood test to diagnose people on track to develop the devastating disease before symptoms arise.

 This study, combined with the results of previous studies, supports the hypothesis that engaging in morning exercise may result in more weight loss compared to engaging in a similar amount of exercise later in the day. Furthermore, we observed individuals who performed most of their exercise sessions in the afternoon or evening tended to have slightly higher levels of EI and reduced NEPA and NEEx, suggesting that there are potentially important differences in the components of energy balance based on time of day exercise is performed.
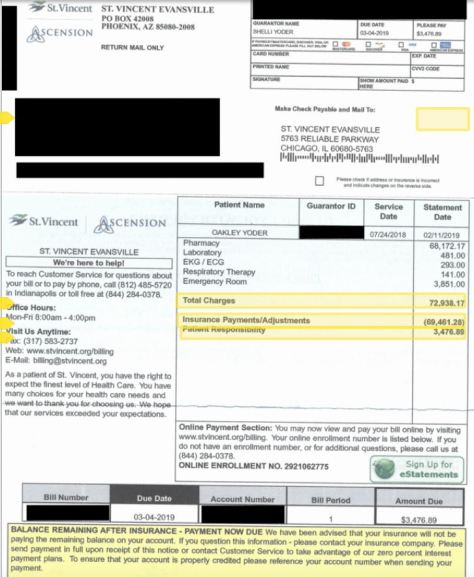
This study, combined with the results of previous studies, supports the hypothesis that engaging in morning exercise may result in more weight loss compared to engaging in a similar amount of exercise later in the day. Furthermore, we observed individuals who performed most of their exercise sessions in the afternoon or evening tended to have slightly higher levels of EI and reduced NEPA and NEEx, suggesting that there are potentially important differences in the components of energy balance based on time of day exercise is performed. “We found staggering inconsistencies between how costs of dementia are calculated across studies and our analysis strongly supports that current estimates fail to recognise the true costs of the diseases, such as Alzheimer’s, that cause dementia. Some studies have estimated that out of pocket expenses for people with dementia are up to one third of their household wealth in the final five years of their life, and that caregivers have healthcare costs that are twice as high as non-caregivers. We also found evidence that costs begin rising up to 10 years prior to diagnosis — we need to better measure and factor all these into future societal cost estimates.”
“We found staggering inconsistencies between how costs of dementia are calculated across studies and our analysis strongly supports that current estimates fail to recognise the true costs of the diseases, such as Alzheimer’s, that cause dementia. Some studies have estimated that out of pocket expenses for people with dementia are up to one third of their household wealth in the final five years of their life, and that caregivers have healthcare costs that are twice as high as non-caregivers. We also found evidence that costs begin rising up to 10 years prior to diagnosis — we need to better measure and factor all these into future societal cost estimates.” “A healthy diet and lifestyle are generally recognized as good for health, but this study is the first large randomized controlled trial to look at whether lifestyle changes actually influence Alzheimer’s disease-related brain changes,” said Susan Landau, a research neuroscientist at Berkeley’s Helen Wills Neuroscience Institute, and principal investigator of the add-on study.
“A healthy diet and lifestyle are generally recognized as good for health, but this study is the first large randomized controlled trial to look at whether lifestyle changes actually influence Alzheimer’s disease-related brain changes,” said Susan Landau, a research neuroscientist at Berkeley’s Helen Wills Neuroscience Institute, and principal investigator of the add-on study.
 PBHWB of 40–42.5 °C was associated with both improved self-rated sleep quality and SE, and when scheduled 1–2 h before bedtime for little as 10 min significant shortening of SOL. These findings are consistent with the mechanism of PBHWB effects being the extent of core body temperature decline achieved by increased blood perfusion to the palms and soles that augments the distal-to-proximal skin temperature gradient to enhance body heat
PBHWB of 40–42.5 °C was associated with both improved self-rated sleep quality and SE, and when scheduled 1–2 h before bedtime for little as 10 min significant shortening of SOL. These findings are consistent with the mechanism of PBHWB effects being the extent of core body temperature decline achieved by increased blood perfusion to the palms and soles that augments the distal-to-proximal skin temperature gradient to enhance body heat 
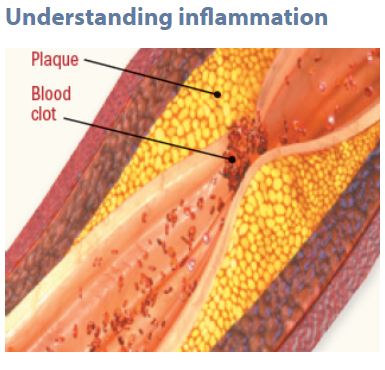 Chronic inflammation often begins with a similar cellular response but morphs into a lingering state that persists far longer. Toxins such as cigarette smoke or an excess of fat cells (especially around the belly area) can also trigger inflammation. So can the fatty plaque inside arteries, which causes inflammatory cells to cover and wall off the plaque from the flowing blood. But the plaque may rupture, mingle with blood, and form a clot. These clots are responsible for the majority of heart attacks and most strokes.
Chronic inflammation often begins with a similar cellular response but morphs into a lingering state that persists far longer. Toxins such as cigarette smoke or an excess of fat cells (especially around the belly area) can also trigger inflammation. So can the fatty plaque inside arteries, which causes inflammatory cells to cover and wall off the plaque from the flowing blood. But the plaque may rupture, mingle with blood, and form a clot. These clots are responsible for the majority of heart attacks and most strokes.