From a ScienceDaily.com online article:
 Now, researchers have developed a fast-acting skin patch that efficiently delivers medication to attack melanoma cells. The device, tested in mice and human skin samples, is an advance toward developing a vaccine to treat melanoma and has widespread applications for other vaccines.
Now, researchers have developed a fast-acting skin patch that efficiently delivers medication to attack melanoma cells. The device, tested in mice and human skin samples, is an advance toward developing a vaccine to treat melanoma and has widespread applications for other vaccines.
Nearly 100,000 new cases of melanoma are diagnosed annually, and 20 Americans die every day from it. Now, researchers have developed a skin patch that efficiently delivers medication within one minute to attack melanoma cells. The device, tested in mice and human skin samples, also could be adapted to deliver other vaccines.
“Our patch has a unique chemical coating and mode of action that allows it to be applied and removed from the skin in just a minute while still delivering a therapeutic dose of drugs,” says Yanpu He, a graduate student who helped develop the device. “Our patches elicit a robust antibody response in living mice and show promise in eliciting a strong immune response in human skin.”
To read more click on the following link: https://www.sciencedaily.com/releases/2019/08/190825075926.htm



 In sarcoidosis, abnormal collections of cells called granulomas invade the organ, interfering with its normal activity and often destroying the surrounding tissue. What is left is a scar, known as fibrosis, dotted with these abnormal granulomas.
In sarcoidosis, abnormal collections of cells called granulomas invade the organ, interfering with its normal activity and often destroying the surrounding tissue. What is left is a scar, known as fibrosis, dotted with these abnormal granulomas.
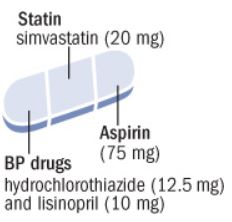 Use of polypill was effective in preventing major cardiovascular events. Medication adherence was high and adverse event numbers were low. The polypill strategy could be considered as an additional effective component in controlling cardiovascular diseases, especially in LMICs.
Use of polypill was effective in preventing major cardiovascular events. Medication adherence was high and adverse event numbers were low. The polypill strategy could be considered as an additional effective component in controlling cardiovascular diseases, especially in LMICs.
 The use of n-3 FA (4 g/d) for improving atherosclerotic cardiovascular disease risk in patients with hypertriglyceridemia is supported by a 25% reduction in major adverse cardiovascular events in REDUCE-IT (Reduction of Cardiovascular Events With EPA Intervention Trial), a randomized placebo-controlled trial of EPA-only in high-risk patients treated with a statin.
The use of n-3 FA (4 g/d) for improving atherosclerotic cardiovascular disease risk in patients with hypertriglyceridemia is supported by a 25% reduction in major adverse cardiovascular events in REDUCE-IT (Reduction of Cardiovascular Events With EPA Intervention Trial), a randomized placebo-controlled trial of EPA-only in high-risk patients treated with a statin.
 This joint position statement from the International Atherosclerosis Society and the International Chair on Cardiometabolic Risk Working Group on Visceral Obesity summarises the evidence for visceral adiposity and ectopic fat as emerging risk factors for type 2 diabetes, atherosclerosis, and cardiovascular disease, with a focus on practical recommendations for health professionals and future directions for research and clinical practice.
This joint position statement from the International Atherosclerosis Society and the International Chair on Cardiometabolic Risk Working Group on Visceral Obesity summarises the evidence for visceral adiposity and ectopic fat as emerging risk factors for type 2 diabetes, atherosclerosis, and cardiovascular disease, with a focus on practical recommendations for health professionals and future directions for research and clinical practice.



 For the study, nearly 8,300 people at risk for heart disease had fasting and nonfasting lipid profile tests done at least four weeks apart. (Fasting means they had nothing to eat or drink except water for at least eight hours before the test.) The differences in their total, LDL, and HDL cholesterol values were negligible. Triglyceride levels were modestly higher in the nonfasting samples.
For the study, nearly 8,300 people at risk for heart disease had fasting and nonfasting lipid profile tests done at least four weeks apart. (Fasting means they had nothing to eat or drink except water for at least eight hours before the test.) The differences in their total, LDL, and HDL cholesterol values were negligible. Triglyceride levels were modestly higher in the nonfasting samples.
 Slower speech, for example, could indicate fatigue or sorrow at one point in time, but over longer periods could signal something more severe, co-founder Jim Harper said.
Slower speech, for example, could indicate fatigue or sorrow at one point in time, but over longer periods could signal something more severe, co-founder Jim Harper said.
 Dr. Grace Dammann, medical director of the Pain Clinic at Laguna Honda Hospital, and seven of her colleagues talk about what does and does not work in the treatment of chronic pain. She talks as both a patient and a provider. There is also a discussion of various non-pharmacologic and complementary medicine modalities to treat pain.
Dr. Grace Dammann, medical director of the Pain Clinic at Laguna Honda Hospital, and seven of her colleagues talk about what does and does not work in the treatment of chronic pain. She talks as both a patient and a provider. There is also a discussion of various non-pharmacologic and complementary medicine modalities to treat pain.

 Antibiotic resistance is a global threat for public health. It is widely acknowledged that antibiotics at sub-inhibitory concentrations are important in disseminating antibiotic resistance via horizontal gene transfer. While there is high use of non-antibiotic human-targeted pharmaceuticals in our societies, the potential contribution of these on the spread of antibiotic resistance has been overlooked so far. Here, we report that commonly consumed non-antibiotic pharmaceuticals, including nonsteroidal anti-inflammatories (ibuprofen, naproxen, diclofenac), a lipid-lowering drug (gemfibrozil), and a β-blocker (propanolol), at clinically and environmentally relevant concentrations, significantly accelerated the conjugation of plasmid-borne antibiotic resistance genes.
Antibiotic resistance is a global threat for public health. It is widely acknowledged that antibiotics at sub-inhibitory concentrations are important in disseminating antibiotic resistance via horizontal gene transfer. While there is high use of non-antibiotic human-targeted pharmaceuticals in our societies, the potential contribution of these on the spread of antibiotic resistance has been overlooked so far. Here, we report that commonly consumed non-antibiotic pharmaceuticals, including nonsteroidal anti-inflammatories (ibuprofen, naproxen, diclofenac), a lipid-lowering drug (gemfibrozil), and a β-blocker (propanolol), at clinically and environmentally relevant concentrations, significantly accelerated the conjugation of plasmid-borne antibiotic resistance genes.