From an MIT Technology Review article (March 11, 2020):
Here are six differences between coronavirus and the flu:
 Coronavirus appears to spread more slowly than the flu. This is probably the biggest difference between the two. The flu has a shorter incubation period (the time it takes for an infected person to show symptoms) and a shorter serial interval (or the time between successive cases). Coronavirus’s serial interval is around five to six days, while flu’s gap between cases is more like three days, the WHO says. So flu still spreads more quickly.
Coronavirus appears to spread more slowly than the flu. This is probably the biggest difference between the two. The flu has a shorter incubation period (the time it takes for an infected person to show symptoms) and a shorter serial interval (or the time between successive cases). Coronavirus’s serial interval is around five to six days, while flu’s gap between cases is more like three days, the WHO says. So flu still spreads more quickly.- Shedding: Viral shedding is what happens when a virus has infected a host, has reproduced, and is now being released into the environment. It is what makes a patient infectious. Some people start shedding the coronavirus within two days of contracting it, and before they show symptoms, although this probably isn’t the main way it is spreading, the WHO says.
- Secondary infections. As if contracting coronavirus wasn’t bad enough, it leads to about two more secondary infections on average. The flu can sometimes cause a secondary infection, usually pneumonia, but it’s rare for a flu patient to get two infections after the flu. The WHO warned that context is key (someone who contracts coronavirus might already have been fighting another condition, for example).
 Don’t blame snotty kids—adults are passing coronavirus around. While kids are the primary culprits for flu transmission, this coronavirus seems to be passed between adults. That also means adults are getting hit hardest—especially those who are older and have underlying medical conditions. Experts are baffled as to why kids seem protected from the worst effects of the coronavirus, according to the Washington Post. Some say they might already have some immunity from other versions of the coronavirus that appear in the common cold; another theory is that kids’ immune systems are always on high alert and might simply be faster than adults’ in battling Covid-19.
Don’t blame snotty kids—adults are passing coronavirus around. While kids are the primary culprits for flu transmission, this coronavirus seems to be passed between adults. That also means adults are getting hit hardest—especially those who are older and have underlying medical conditions. Experts are baffled as to why kids seem protected from the worst effects of the coronavirus, according to the Washington Post. Some say they might already have some immunity from other versions of the coronavirus that appear in the common cold; another theory is that kids’ immune systems are always on high alert and might simply be faster than adults’ in battling Covid-19.- Coronavirus is far deadlier than the flu. Thus far, the mortality rate for coronavirus (the number of reported cases divided by the number of deaths) is around 3% to 4%, although it’s likely to be lower because many cases have not yet been reported. The flu’s rate is 0.1%.
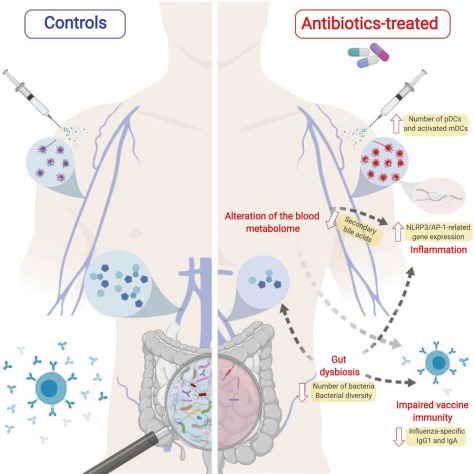
- There is no cure or vaccine for the coronavirus. Not yet, anyway, although work is under way. There is, however, a flu vaccine—and everyone should get it, not least because being vaccinated could help lessen the load on overstretched medical services in the coming weeks.



 Although coronavirus disease 2019 (COVID-19) dominates the news in early 2020, it affects few people in the US. In contrast, at the same time the US is experiencing a severe influenza epidemic, which has caused an estimated 250 000 hospitalizations and 14 000 deaths.
Although coronavirus disease 2019 (COVID-19) dominates the news in early 2020, it affects few people in the US. In contrast, at the same time the US is experiencing a severe influenza epidemic, which has caused an estimated 250 000 hospitalizations and 14 000 deaths.