From a The BMJ Views and Reviews article by David Oliver (February 5, 2020):
 Last year the Lancet published a paper on the impact of wearing gowns, surveying 928 adult patients and carrying out structured interviews with 10 patients. Over half (58%) reported wearing the gown despite feeling uncertain that it was a medical necessity. Gown design was considered inadequate, with 61% reporting that they struggled to put it on or required assistance and 67% reporting that it didn’t fit. Most worryingly, 72% felt exposed, 60% felt self-conscious, and 57% felt uncomfortable wearing the gown.
Last year the Lancet published a paper on the impact of wearing gowns, surveying 928 adult patients and carrying out structured interviews with 10 patients. Over half (58%) reported wearing the gown despite feeling uncertain that it was a medical necessity. Gown design was considered inadequate, with 61% reporting that they struggled to put it on or required assistance and 67% reporting that it didn’t fit. Most worryingly, 72% felt exposed, 60% felt self-conscious, and 57% felt uncomfortable wearing the gown.
I’ve often wondered why on earth we routinely put so many patients into hospital gowns within minutes of their arrival at hospital.
Sometimes referred to as “dignity gowns,” such dignity as they afford is only in comparison to being stark naked. They don’t come in a wide range of sizes or lengths, and they’re open along the back. You tend to get what you’re given and make do. The effect is to leave patients with lots of exposed flesh, with underwear or buttocks intermittently displayed and a feeling of extreme vulnerability, not to mention being cold if they have no other layers to wear.



 In this video, best-selling author Abraham Verghese, MD, discusses the origins of the study he coauthored identifying 5 practices that foster meaningful connections between physicians and patients.
In this video, best-selling author Abraham Verghese, MD, discusses the origins of the study he coauthored identifying 5 practices that foster meaningful connections between physicians and patients.
 The proportion of patients who have two or more medical conditions simultaneously is, however, rising steadily. This is currently termed multimorbidity, although patient groups prefer the more intuitive “multiple health conditions.” In high income countries, multimorbidity is mainly driven by age, and the proportion of the population living with two or more diseases is steadily increasing because of demographic change. This trend will continue.
The proportion of patients who have two or more medical conditions simultaneously is, however, rising steadily. This is currently termed multimorbidity, although patient groups prefer the more intuitive “multiple health conditions.” In high income countries, multimorbidity is mainly driven by age, and the proportion of the population living with two or more diseases is steadily increasing because of demographic change. This trend will continue.


 The
The 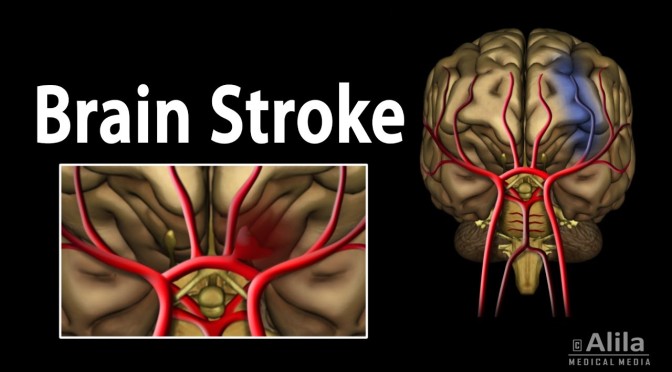
 As a consultant, I had profoundly failed to appreciate the experience of fatigue and apathy among patients. More than excessive tiredness, the fatigue was overwhelming, turning simple activities into insurmountable, exhausting challenges. It was frustrating and I fell into the trap of overexertion when I did have energy, thus exhausting myself and sabotaging the day’s recovery plan. Had staff not been so adept at encouraging me when I lacked energy and holding me back when I tried to overdo things, I would have squandered much valuable rehabilitation time.
As a consultant, I had profoundly failed to appreciate the experience of fatigue and apathy among patients. More than excessive tiredness, the fatigue was overwhelming, turning simple activities into insurmountable, exhausting challenges. It was frustrating and I fell into the trap of overexertion when I did have energy, thus exhausting myself and sabotaging the day’s recovery plan. Had staff not been so adept at encouraging me when I lacked energy and holding me back when I tried to overdo things, I would have squandered much valuable rehabilitation time. 
 The top 10 most commonly administered antibiotics in the ER for nonadmitted patients were:
The top 10 most commonly administered antibiotics in the ER for nonadmitted patients were:
 Vim’s solution curates top providers and pairs patients with those providers, leveraging a combination of online booking and referral coordination. On the provider side, it
Vim’s solution curates top providers and pairs patients with those providers, leveraging a combination of online booking and referral coordination. On the provider side, it  Vim says it has access to 10,000,000 patient profiles and 150,000 providers through major U.S.-based health plan partners. In the next 12 months, it loftily intends to “meaningfully reduce” the $1 trillion of excess cost in health care in the U.S. by targeting inconsistencies in treatment.
Vim says it has access to 10,000,000 patient profiles and 150,000 providers through major U.S.-based health plan partners. In the next 12 months, it loftily intends to “meaningfully reduce” the $1 trillion of excess cost in health care in the U.S. by targeting inconsistencies in treatment.
 Zing’s plan will give seniors access to a network of clinics in Cook County, Illinois, starting in January. The company hopes to expand to three states by 2022. It’s a managed care plan, which means the Centers for Medicare and Medicaid Services (CMS) will pay a single monthly fee per member in exchange for a more holistic approach to nurturing patient health. Zing is working with a network of community health centers, including Oak Street Health, which recently raised $65 million for its senior-focused facilities.
Zing’s plan will give seniors access to a network of clinics in Cook County, Illinois, starting in January. The company hopes to expand to three states by 2022. It’s a managed care plan, which means the Centers for Medicare and Medicaid Services (CMS) will pay a single monthly fee per member in exchange for a more holistic approach to nurturing patient health. Zing is working with a network of community health centers, including Oak Street Health, which recently raised $65 million for its senior-focused facilities.