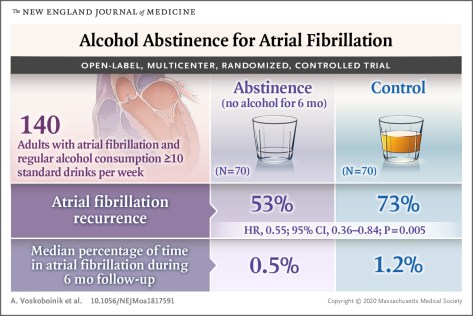
Abstinence from alcohol reduced arrhythmia recurrences in regular drinkers with atrial fibrillation.
January 2, 2020 Atrial fibrillation is the most common sustained arrhythmia,1 and alcohol is consumed by a majority of U.S. adults.2 The current study showed that among regular drinkers, a substantial reduction in alcohol consumption by patients with symptomatic atrial fibrillation was associated with a reduction in recurrence of atrial fibrillation and a reduced proportion of time spent in atrial fibrillation. Earlier meta-analyses showed that alcohol was associated with a dose-related increased risk of incident atrial fibrillation, with increased risk observed even among drinkers who consumed as few as 7 drinks per week.8 Current trends show a rise in alcohol consumption among adults older than 60 years of age,2coupled with greater prevalence of atrial fibrillation in this age group. The present study, with participants having an average intake of approximately 17 drinks per week at baseline, suggests that consumption at these levels may contribute to atrial fibrillation.


 It was all horribly familiar — a rerun of an episode 15 months earlier, when she was with her family in River Vale, N.J. Back then, the burning pressure sent her to the emergency department, and she was told the same thing: She was having a heart attack. Immediately the cardiologist looked for blockages in the coronary arteries, which feed blood and oxygen to the hardworking muscles of her heart. That was the cause of most heart attacks. But they found no blockage.
It was all horribly familiar — a rerun of an episode 15 months earlier, when she was with her family in River Vale, N.J. Back then, the burning pressure sent her to the emergency department, and she was told the same thing: She was having a heart attack. Immediately the cardiologist looked for blockages in the coronary arteries, which feed blood and oxygen to the hardworking muscles of her heart. That was the cause of most heart attacks. But they found no blockage. Indeed, that was the clue that led the rheumatologist to a likely diagnosis: Behcet’s disease. It’s an unusual inflammatory disorder characterized by joint pains, muscle pains and recurrent ulcers in mucus membranes throughout the body. Almost any part of the body can be involved — the eyes, the nose and lungs, the brain, the blood vessels, even the heart. Behcet’s was named after a Turkish dermatologist who in 1937 described a triad of clinical findings including canker sores (medically known as aphthous ulcers), genital ulcers and an inflammatory condition of the eye.
Indeed, that was the clue that led the rheumatologist to a likely diagnosis: Behcet’s disease. It’s an unusual inflammatory disorder characterized by joint pains, muscle pains and recurrent ulcers in mucus membranes throughout the body. Almost any part of the body can be involved — the eyes, the nose and lungs, the brain, the blood vessels, even the heart. Behcet’s was named after a Turkish dermatologist who in 1937 described a triad of clinical findings including canker sores (medically known as aphthous ulcers), genital ulcers and an inflammatory condition of the eye.
 Researchers matched 7,743 people with osteoarthritis with 23,229 healthy people who rarely or never took NSAIDs. People with osteoarthritis had a 42% higher risk of heart failure and a 17% higher risk of coronary artery disease compared with healthy people. After controlling for a range of factors that contribute to heart disease (including high body mass index, high blood pressure, and diabetes), they concluded that 41% of the increased risk of heart disease related to osteoarthritis was due to the use of NSAIDs.
Researchers matched 7,743 people with osteoarthritis with 23,229 healthy people who rarely or never took NSAIDs. People with osteoarthritis had a 42% higher risk of heart failure and a 17% higher risk of coronary artery disease compared with healthy people. After controlling for a range of factors that contribute to heart disease (including high body mass index, high blood pressure, and diabetes), they concluded that 41% of the increased risk of heart disease related to osteoarthritis was due to the use of NSAIDs.
 Costochondritis is caused by inflammation of the cartilage between the ribs and the breastbone, called the costosternal joints (see illustration). This uncommon condition can trigger a stabbing, aching pain that’s often mistaken for a heart attack.
Costochondritis is caused by inflammation of the cartilage between the ribs and the breastbone, called the costosternal joints (see illustration). This uncommon condition can trigger a stabbing, aching pain that’s often mistaken for a heart attack.