From a Science Magazine online article:
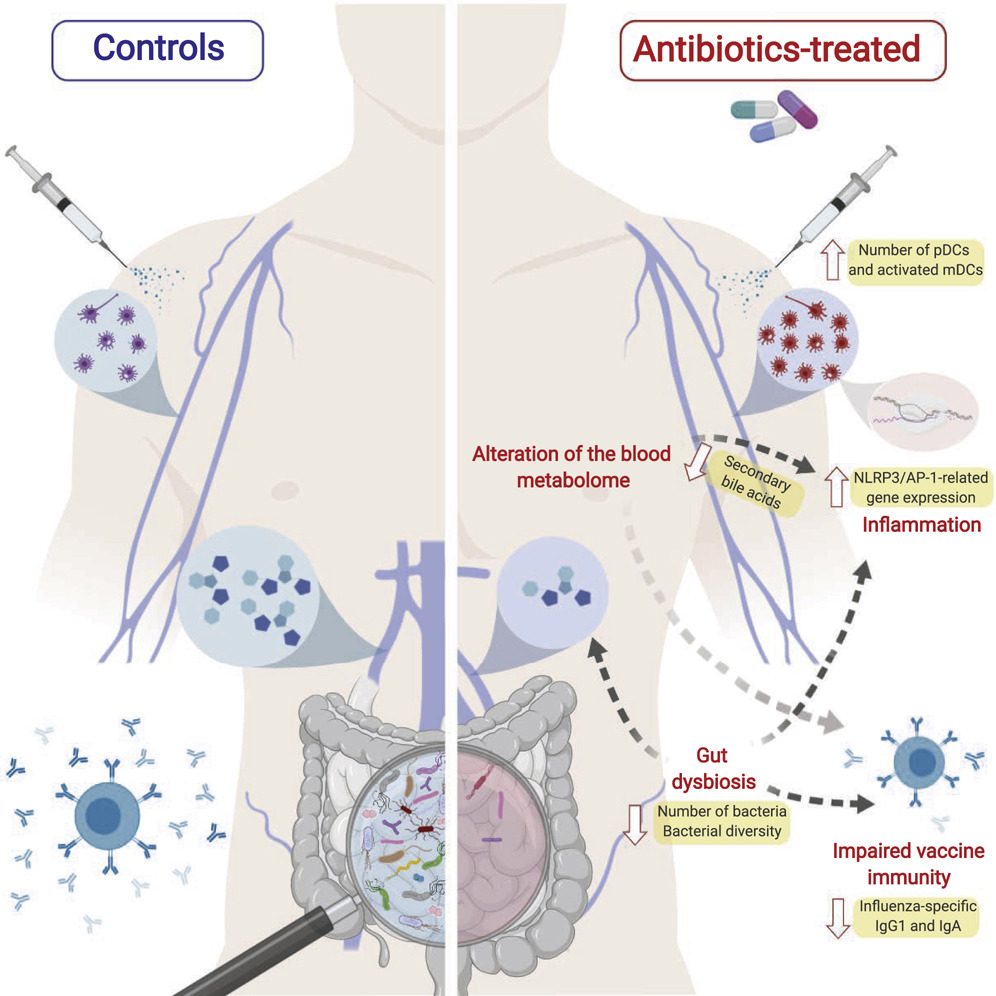
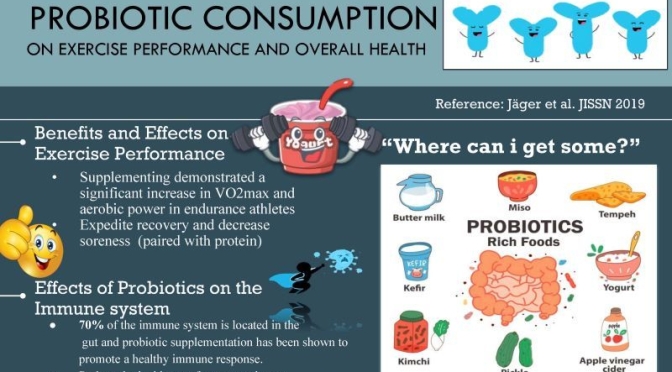
Antibiotic use diminished the gut microbiome composition and impaired the ability of the immune system to generate antibodies. Treatment with antibiotics also disturbed bile acid metabolism and caused inflammatory responses.
From the original findings the Journal “Cell.com”:
Emerging evidence indicates a central role for the microbiome in immunity. However, causal evidence in humans is sparse. Here, we administered broad-spectrum antibiotics to healthy adults prior and subsequent to seasonal influenza vaccination. Despite a 10,000-fold reduction in gut bacterial load and long-lasting diminution in bacterial diversity, antibody responses were not significantly affected. However, in a second trial of subjects with low pre-existing antibody titers, there was significant impairment in H1N1-specific neutralization and binding IgG1 and IgA responses.
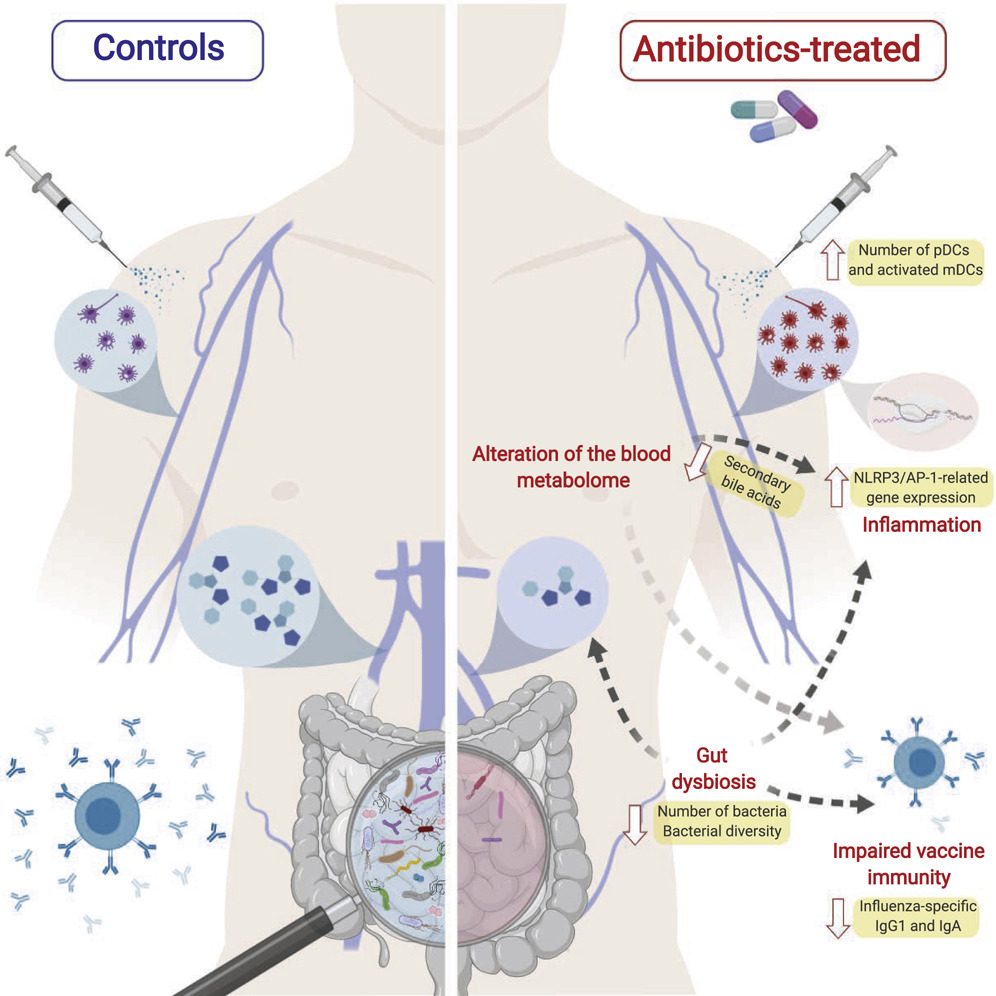
In addition, in both studies antibiotics treatment resulted in (1) enhanced inflammatory signatures (including AP-1/NR4A expression), observed previously in the elderly, and increased dendritic cell activation; (2) divergent metabolic trajectories, with a 1,000-fold reduction in serum secondary bile acids, which was highly correlated with AP-1/NR4A signaling and inflammasome activation. Multi-omics integration revealed significant associations between bacterial species and metabolic phenotypes, highlighting a key role for the microbiome in modulating human immunity.




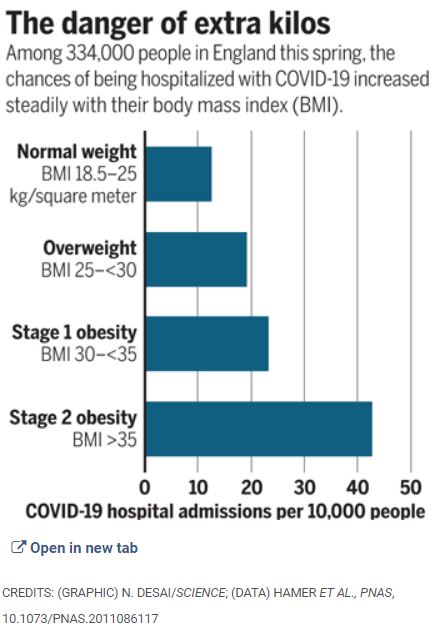



 As states grapple with the question of when it will be safe to reopen businesses and relax social distancing, there’s increasing urgency to better understand who’s immune to Covid-19. Does having the virus and recovering mean you can’t get it again, or at least that you can’t be reinfected for some time?
As states grapple with the question of when it will be safe to reopen businesses and relax social distancing, there’s increasing urgency to better understand who’s immune to Covid-19. Does having the virus and recovering mean you can’t get it again, or at least that you can’t be reinfected for some time?